Risk Factors in Substance Abuse Relapse: Mental Health Risk Factors
There are many risk factors that can become triggers that can lead to relapse. In this article we will cover how mental health, such as depression and anxiety, can be the cause of addition and relapse. We will also discuss how learning coping skills during treatment can lead to a successful recovery.
Addiction & Relapse
Addiction is a disease that can be treated with the help of medical professionals.1 It is a chronic disease that affects the brain and is influenced by a person’s genetics, their environment, and their individual life experiences.1
Relapse is when a person has returned to abusing substances after a period of not using.2 It is common and happens to many people that are recovering from a substance use disorder. 2 It is important to know what to do and how to get help after a relapse. Going to treatment and continuing your recovery by attending aftercare and support groups has helped many people remain sober.
Take Our Substance Abuse Self-Assessment
Take our free, 5-minute substance abuse self-assessment below if you think you or someone you love might be struggling with substance abuse. The evaluation consists of 11 yes or no questions that are intended to be used as an informational tool to assess the severity and probability of a substance use disorder. The test is free, confidential, and no personal information is needed to receive the result.
What is the Connection Between Mental Health and Addiction?

There are several hypotheses to explain why depression, anxiety and addiction often occur together. One possibility is that they share common risk factors.3 For instance, certain genetic differences can influence the likelihood of developing both substance use disorders and mental illness.3 Even environmental factors, such as previous exposure to trauma or significant stress, can result in lasting epigenetic changes that can contribute to the development of both of these conditions.3
These experiences might also make a person more vulnerable to using substances to cope.3 Studies have estimated that half of all people with a mental health disorder will also develop a substance abuse disorder, and vice versa.4
When a person has both mental health issues and addiction, you may see several different types of symptoms, which can depend on the type of mental health disorder involved. In general, if someone has an addiction, regardless of the presence of a mental health disorder, you will see some or even all of the following symptoms:5
- Being unable to take care of responsibilities at home, work, or school.
- Cravings for a substance.
- Giving up leisure activities or hobbies to use substances.
- Increased interpersonal conflict with others around their use of substances.
- Spending significant amounts of time and money seeking substances, using them, and recovering from using.
- Taking more of a drug than intended.
- The development of tolerance, which means needing more and more of a substance to achieve the same effects as before.
- Unsuccessful attempts to cut back on use.
- Using in risky situations.
- Using substances even though they know it is making a mental or physical condition worse.
Signs of mental illness can include many types of behaviors, but commonly include:6
- Changes in appetite.
- Changes in sex drive.
- Changes in sleep patterns.
- Excessive worry or fears.
- Extreme changes in mood, between excitement and depression.
- Feeling various aches, pains, and symptoms of various vague illnesses.
- Inability to think clearly or focus.
- Isolating from others.
- Prolonged feelings of anger.
- Sadness that lasts for several days.
- Suicidal thoughts or plans.
- Unable to fulfill normal responsibilities at home or work.
Regardless of the factors that led to the development of an addiction, it can be treated. Experiencing trauma and stress are often contributing factors to the development of a substance use disorder. Among veterans with PTSD, 1 in 5 also has a substance abuse disorder.3
Regardless of what led to your or a loved one’s addiction, American Addiction Centers (AAC) offers addiction treatment for those with a co-occurring disorder. Call us today at
Depression and Substance Abuse
Depression is a common form of mental illness, and it is more than just feelings of sadness. People with depression may experience feelings of hopelessness throughout the day for at least 2 weeks. Other symptoms include: 7
- Feeling helpless or hopeless.
- Lack of motivation or pleasure in actives.
- Changes in appetite and weight.
- Feeling restless or irritable.
- Decrease in energy.
- Physical discomforts such as body aches or pains, headaches, and digestive problems.
At times, people will use substances to try to cope with negative thoughts. Among people with depression, alcohol abuse is common, though all types of substances may be abused, including benzodiazepines, marijuana, stimulants, and opioids. Around 40% of people who have depression also have a substance use disorder.8
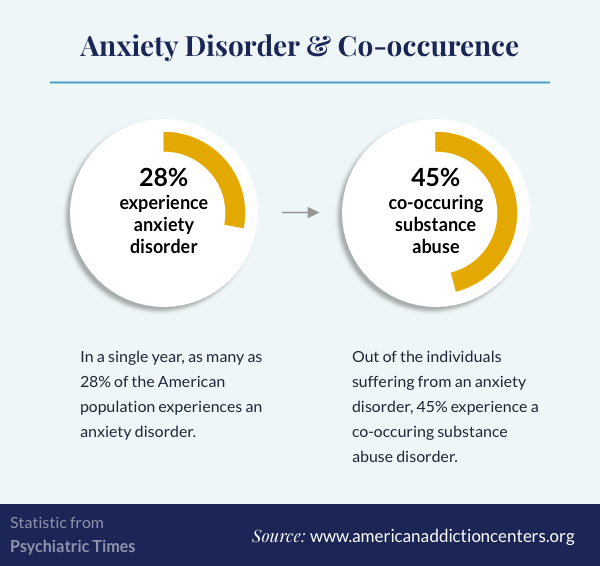
Anxiety and Substance Abuse
Anxiety can take many forms, including generalized anxiety disorder, social anxiety, and panic attacks. Everyone has anxious moments, but with anxiety disorders, the feelings of worry never goes away.9 Anxiety permeates a person’s thoughts and can impair daily functions. With anxiety, people usually:9
- Becoming irritable.
- Experience muscle tension.
- Feel restless and unable to settle down or relax.
- Get tired easily.
- Have problems concentrating.
- Struggle to control worry.
When a person has a panic disorder, they may feel as if they are going to die. They can also experience:
- A pounding heartbeat or accelerated heartrate.
- Sweating.
- Shaking or trembling.
- Shortness of breath.
- Feeling they have lost control.
People with panic attacks become so afraid of having another one that they change their lives to avoid anything that might trigger an attack, such as leaving home or being in a crowd.9
A person with social anxiety will be overwhelmed by social interactions and feel unable to interact in routine situations.9 Their fears of being judged or disliked can become so intense that they avoid social interactions.9
People with social anxiety, generalized anxiety, or panic disorder often turn to substances to help control their anxiety. In about 75% of cases, anxiety appears before a substance abuse disorder, but over time, the 2 disorders fuel one another in a vicious cycle.10
Preventing Addiction Relapse
In treatment, you learn coping skills to help manage your addiction, anxiety, depression, and other mental health disorders. However, as you return to daily life, it is important that you continue to regularly focus on the skills you learned in treatment so you do not relapse into active addiction.
Mutual help groups such as 12-step programs or other peer support groups have been strongly associated with preventing relapse. These groups include: 11, 12
- Narcotics Anonymous (NA), a 12-step program for people recovering from drug addiction.
- Alcoholics Anonymous (AA), a 12-step program for people recovering from alcohol use disorders.
- SMART recovery, a support group that does not use a spiritually based 12-step model, which may be better for people who are not comfortable with spirituality.
- AAC offers free virtual support meetings if you are unable to attend live groups.
Attending these groups, or similar groups, can both help prevent relapse as well as reduce symptoms of anxiety and depression.11, 13 It can be especially hard to maintain your recovery when you are also dealing with anxiety, depression, or other mental disorders. 11, 13 If your mental health disorder is not being managed appropriately, you could easily turn back to drugs or alcohol to cope, creating a vicious cycle.14 Various therapies can help manage addiction recovery, including mindfulness therapy.
Preventing Relapse Through Mindfulness
Mindfulness therapy is a somewhat new intervention to help people in recovery. It combines such techniques as breathing exercises and meditation, with Cognitive Behavioral Therapy (CBT).
Mindfulness meditation acts as a replace prevention; helping to increase understanding of how negative emotions feed into the craving for drugs or alcohol and better alternatives for coping.15 A person who is struggling with mental health issues and addiction can use mindfulness therapy techniques to practice alternative behaviors when they want to use substances.
A recent study found that mindfulness-based relapse prevention can be used effectively to help those with a substance use disorder, both with and without additional depression and anxiety symptoms.16
Integrated Treatment for Co-occurring Substance Use and Mental Health Disorders
Substance use disorders and mental health issues are common co-occurrences.17 Just because you experience symptoms of depression or anxiety doesn’t necessarily mean that you, or a loved one, has a mental health disorder.17 Research has found that depressive thoughts can be strongly linked with substance use cravings.18
One of the most frequently asked questions about co-occurring disorders is whether the substance abuse or mental illness came first. The answer isn’t always easy to discern. However, regardless of whether one preceded the other, or if both arise independently, an integrated treatment model can effectively and simultaneously manage both.19
It can be difficult to find a treatment provider who understands both mental health disorders and addiction. Integrated treatment, which addresses substance abuse and mental health care simultaneously, has been shown to be superior to treatment that focuses on addiction and mental health separately.19, 20
AAC is one of the leading providers of substance abuse treatment, with facilities across the United States. AAC offers integrated treatment, which can address your mental health and substance abuse needs in one program. Give us a call today to learn more about our treatment programs and how AAC can help you with your addiction and co-occurring mental health issues.
Integrated treatment, which addresses co-occurring diagnoses together, is more effective than treating disorders separately.19 Although treating both a mental health disorder and a substance abuse disorder is challenging, many people learn to manage their co-occurring disorders with the right support and treatment. Finding the best treatment program for you and getting started today is the first step in your journey.
Sources:
- American Society of Addiction Medicine. (2019) Definition of Addiction.
- NIDA: Drug Facts. What is a relapse?
- NIDA. (2020). Why is there comorbidity between substance use disorders and mental illnesses?
- NIDA. (2020). Comorbidity: Substance Use Disorders and Other Mental Illnesses DrugFacts.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA.
- NAMI. (2020). Warning signs and symptoms.
- National Institutes on Mental Health. (2016). Depression basics.
- Brenner, P., Brandt, L., Li, G., DiBernardo, A., Bodén, R., & Reutfors, J. (2020). Substance use disorders and risk for treatment resistant depression: a population-based, nested case-control study. Addiction, 115(4), 768–777.
- National Institute on Mental Health. Anxiety disorders.
- Smith, J. P., & Book, S. W. (2008). Anxiety and substance use disorders: A review. The Psychiatric Times, 25(10), 19–23.
- Wilcox, C. E., & Tonigan, J. S. (2018). Changes in depression mediate the effects of AA attendance on alcohol use outcomes. The American journal of drug and alcohol abuse, 44(1), 103–112.
- Kelly JF, Stout R, Zywiak W, Schneider R. A 3-year study of addiction mutual-help group participation following intensive outpatient treatment. Alcohol Clin Exp Res. 2006;30(8):1381-1392.
- Timko C, Cronkite RC, McKellar J, Zemore S, Moos RH. Dually diagnosed patients’ benefits of mutual-help groups and the role of social anxiety. J Subst Abuse Treat. 2013;44(2):216-223.
- Sliedrecht W, de Waart R, Witkiewitz K, Roozen HG. Alcohol use disorder relapse factors: A systematic review. Psychiatry Res. 2019;278:97-115.
- Grant, S., Colaiaco, B., Motala, A., Shanman, R., Booth, M., Sorbero, M., & Hempel, S. (2017). Mindfulness-based Relapse Prevention for Substance Use Disorders: A Systematic Review and Meta-analysis. Journal of addiction medicine, 11(5), 386–396.
- Roos, C. R., Bowen, S., & Witkiewitz, K. (2017). Baseline patterns of substance use disorder severity and depression and anxiety symptoms moderate the efficacy of mindfulness-based relapse prevention. Journal of consulting and clinical psychology, 85(11), 1041–1051.
- ASAM (2010)A Description of Addiction.
- Witkiewitz, K., & Bowen, S. (2010). Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of consulting and clinical psychology, 78(3), 362–374.
- Substance Abuse and Mental Health Treatment Services Administration. (2015). TIP 45: Detoxification and Substance Abuse Treatment.
- National Institute on Drug Abuse. (2020). What are the treatments for comorbid substance use disorder and mental health conditions?

