Borderline Personality Disorder (BPD): Causes, Types & Treatment
Borderline Personality Disorder (BPD) is a mental health disorder characterized by dramatic and/or eccentric emotional responses and behaviors such as unstable moods that can affect relationships with others.
What is a Personality?
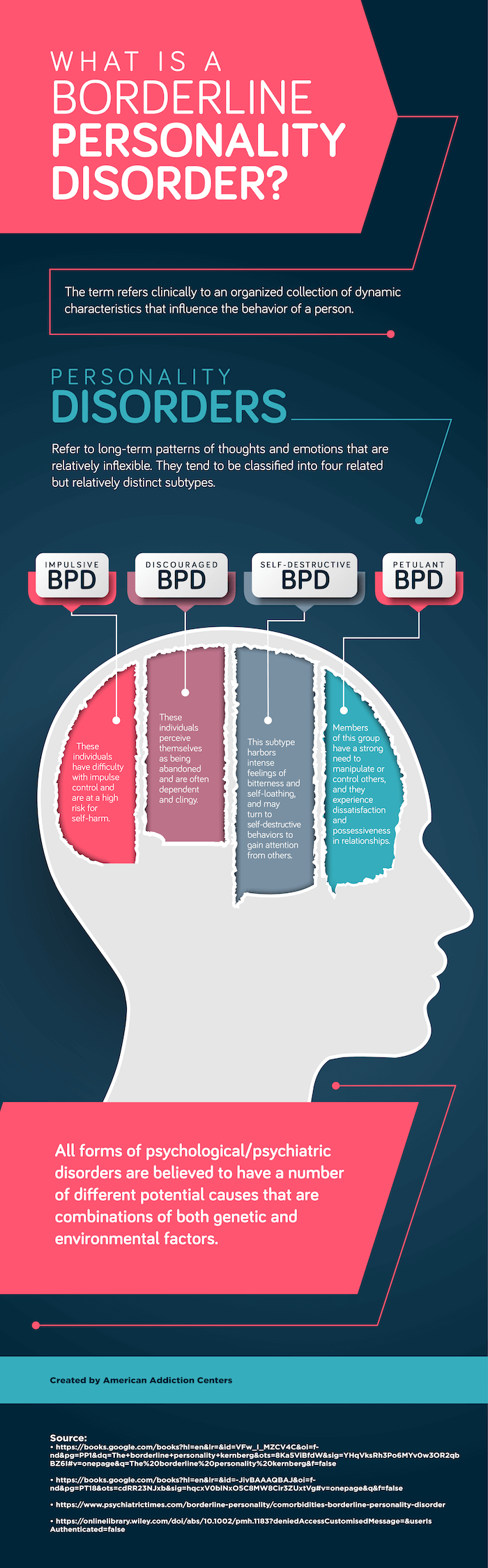
The term personality is used in a number of different contexts; however, according to The Encyclopedia of Psychology it refers clinically to an organized collection of dynamic characteristics that influence the behavior of a person.
These dynamic characteristics contribute to the way the person acts, feels, and thinks. They reflect and influence nearly every aspect of the individual’s behavior. Thus, the clinical concept of personality indicates that it is something that is relatively stable (emphasis on the term relatively), it has a function, and it has to actually do something.
 When personality theorists imply that personality must do something, they mean that the personality must function to define the person’s motivations, express their needs, guide their relationships, and guide other behaviors. One of the most enduring traits in the study of personality is the notion of extraversion that suggests that individuals with this trait tend to be relatively sociable and outgoing as opposed to being withdrawn and reserved. If a personality theorist or clinician describes someone as “an extrovert,” this description communicates something about that person and allows relatively reliable assumptions to be made about how the person will normally act in most situations.
When personality theorists imply that personality must do something, they mean that the personality must function to define the person’s motivations, express their needs, guide their relationships, and guide other behaviors. One of the most enduring traits in the study of personality is the notion of extraversion that suggests that individuals with this trait tend to be relatively sociable and outgoing as opposed to being withdrawn and reserved. If a personality theorist or clinician describes someone as “an extrovert,” this description communicates something about that person and allows relatively reliable assumptions to be made about how the person will normally act in most situations.
However, personality descriptions are best applied in overall general terms; they are much less descriptive in specific instances. If an individual is observed, and their behavior recorded over many different situations over a significant period of time, there will be certain general enduring patterns of behavior that will occur that should be consistent with general themes regarding the person’s personality. An extrovert will be outgoing and sociable far more often than not; however, they may not always be outgoing and sociable in every situation. People often control their actions to fit the situation. Personality researchers and clinicians understand this apparent discrepancy and realize that there is no specific general description of anyone that will apply in every single instance.
Personality Disorders
 Personality disorders represent enduring patterns of behavior and inner experiences, such as emotions that are relatively inflexible (meaning that they are prone to be expressed in situations where an individual would normally temper certain aspects of their behavior), pervasive (meaning they occur in many different situations), are significant departures from expectations of a person’s social environment or culture, and appeared early in the development of the individual and continue to be expressed over time as the person matures. These enduring patterns of behavior are often dysfunctional and result in significant distress to the individual and/or to others with whom the individual interacts.
Personality disorders represent enduring patterns of behavior and inner experiences, such as emotions that are relatively inflexible (meaning that they are prone to be expressed in situations where an individual would normally temper certain aspects of their behavior), pervasive (meaning they occur in many different situations), are significant departures from expectations of a person’s social environment or culture, and appeared early in the development of the individual and continue to be expressed over time as the person matures. These enduring patterns of behavior are often dysfunctional and result in significant distress to the individual and/or to others with whom the individual interacts.
Thus, personality disorders:
- Are stable tendencies toward feeling and behaving that have endured since early childhood or adolescence
- Are in conflict with the normal expectations of the individual’s social environment or culture
- Lead to significant issues regarding the individual’s ability to function in society and negatively affect the person’s relationships, occupation, goals, and overall level of functioning
Since personality disorders are relatively enduring (have been present since childhood and continued) and stable (are relatively resistant to different expectations in different situations), the behaviors associated with them cannot be better explained by the use of medications or drugs, specific time-limited reactions to stress or other events, or as a result of the effect of some other medical condition, such as a head injury, stroke, etc. If other explanations for the particular behaviors observed in people suspected of having a personality disorder exist, then the people are most likely not expressing symptoms of a personality disorder.
In the current diagnostic scheme for psychiatric/psychological disorders, The Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition (DSM-5), the categories of personality disorders remain relatively unchanged from previous editions, despite harsh criticisms of the diagnostic criteria of the overall scheme used by the American Psychiatric Association’s methods at classifying these disorders. The large number of overlapping diagnostic criteria for the nine different personality disorders, despite the notion in the DSM that personality disorders each represent discrete entities, as well as the observation that the same personality disorder diagnosed in two different individuals may have totally different presentations, have fueled these criticisms. Nonetheless, it appears that the current diagnostic scheme regarding personality disorders will remain unchanged for quite some time.
Borderline Personality Disorder (BPD)
The nine personality disorders in the DSM-5 are further grouped into three major clusters of disorders, such that each cluster is based on the major feature that defines the behavior observed in those personality disorders. Borderline personality disorder is one of four personality disorders belonging to a group of personality disorders where dramatic and/or very eccentric emotional responses are the major personality features/characteristics that drive the person’s overall behavior.
The notion of borderline personality disorder was extant long before the development of the DSM series. Individuals diagnosed with borderline personality disorder have long been believed to be straddling on the edge of “normal” and psychosis (a loss of the notion of reality).
Symptoms & Diagnosis of Borderline Personality Disorder
According to the American Psychiatric Association (APA), there are nine potential symptoms that can occur in individuals who are diagnosed with borderline personality disorder (BPD). In order to receive a formal diagnosis of BPD, an individual would have to satisfy or meet at least five of the nine diagnostic criteria (diagnostic criteria are synonymous to signs or symptoms). The general symptoms of borderline personality disorder include:
- A significant and persistently unstable sense of self
- Desperate efforts to avoid being abandoned (These can be efforts to avoid real situations where the individual feels that they will be abandoned or situations that they imagine can occur that will result in them being abandoned.)
- Long-term feelings of loneliness or emotional emptiness
- A long-term pattern of alternating between totally idealizing other people to totally devaluating them (In clinical terms, this is often referred to as splitting: The individual totally idolizes a person; then, when the person does something that offends them, they totally demonize the same person. Individuals engaging in splitting seem to have no middle ground.)
- The demonstration of a severe impulsivity that occurs in at least two areas of behavior and is potentially self-injurious or self-damaging (e.g., substance abuse, binge eating, multiple sexual contacts, etc.)
- Repeated gestures at suicide, threats of committing suicide, or even repeated actual attempts at suicide
- Engaging in various forms of self-mutilating behavior, such as cutting or burning oneself with a lighter
- Demonstrating multiple significant unstable emotional outbursts
- Paranoid thoughts or severe dissociative experiences, such as being removed or detached from reality, having severe amnestic events, or feeling as if one is detached from one’s body
Because the diagnostic criteria indicate that one must satisfy five of the nine total criteria, there are literally many different ways that BPD can present itself in individuals. For example, there are over 100 different five-symptom combinations possible. Of course, individuals can also have more than five symptoms, so there are many other combinations of six, seven, or eight criteria, as well as individuals with severe presentations who may fit all nine diagnostic criteria. This means that BPD can present in a number of different ways.
Otto Kernberg, a psychiatrist who specialized in understanding personality disorders, believed that the pervasive feelings of loneliness and the need to belong to something were the driving forces behind all of the other behaviors associated with BPD. Other attempts to refine the diagnosis and define different subtypes of BPD have been attempted. Perhaps the most enduring of the attempts to define different BPD subtypes comes from the personality psychologist Theodore Millon.
BPD Subtypes
Millon classified BPD subtypes by the general pattern of their overall pathology. This resulted in four related, but relatively distinct, subtypes of BPD:
- Impulsive BPD: The major feature in this subtype is difficulty with impulse control. These individuals are at a high risk for self-harm, including attempts at suicide, and they often become engaged in thrill-seeking activities.
- Discouraged BPD: This subtype is very dependent on others and thus very needy and clingy. These individuals often present as being very passive until they perceive themselves as being abandoned. Once they feel abandoned, issues with anger control and emotional stability surface. Although they are dependent and clingy, any amount of attention will not satisfy them.
- Self-destructive BPD: This subtype harbors intense feelings of bitterness and self-hatred. They attempt to find comfort in getting attention from others, and if this need is not satisfied (and it never is for long), they may turn to self-destructive behaviors, including suicidal threats or attempts, substance abuse, and potentially destructive thrill-seeking.
- Petulant BPD: This subtype fluctuates between outbursts of explosive anger and feelings of being unworthy or unloved. They have a strong need to manipulate or control others, and they become very possessive, which results in extreme dissatisfaction in their relationships. This leads to issues with substance abuse and other potential damaging issues.
Many of the other classifications of the subtypes of BPD are similar to Millon’s but may combine one or two of the different subtypes. In addition, the observation made by Kernberg above – that the driving force behind BPD was one of loneliness and needing to belong – appears to be an important feature in all of the subtypes mentioned by Millon.
Causes of BPD
The vast majority of recognized forms of mental illness or psychiatric/psychological disorders have no known formal cause. Instead, there are a number of different associations noted with these disorders that may contribute to their development; however, no formal causal relationship has ever been established between any specific factor, including genetic associations, a history of abuse, certain other personality characteristics, or other environmental factors and any personality disorder.
BPD Rarely Occurs in Isolation
The term comorbidity is used by clinicians to describe a situation where a person is diagnosed with more than one type of disorder at the same time. The terms dual diagnosis or co-occurring disorders are now often used to specify a situation where an individual has a mental health disorder that is comorbid with a substance use disorder. Because BPD is a severe disorder with extensive psychopathology, it is commonly comorbid with several other types of disorders. The most common disorders comorbid with BPD include the following:
- Major depressive disorder, often referred to as just clinical depression or depression, is the most common comorbid disorder diagnosed with BPD. As one might expect the severe feelings of emptiness, loneliness, fear of abandonment, and other behaviors associated with BPD often lead to severe feelings of depression.
- Anxiety disorders, such as panic disorders (the occurrence of multiple panic attacks) and phobias (unrealistic fears of situations or objects), are also frequently comorbid with BPD.
- BPD is often comorbid with bipolar disorder, which is a severe disorder where individuals vacillate between extreme presentations of depression and mania.
- Post-traumatic stress disorder is often comorbid with BPD due to a combination of the extreme emotional liability these individuals experience and of having a history of abuse as children, their tendency to get involved in relationships that are abusive and dysfunctional, or their vulnerability to be victims of aggressive types of crimes.
- Substance use disorders are very often comorbid with BPD as mentioned above. The tendency to engage in substance abuse is a result of a number of different factors for individuals with BPD, including their penchant for self-destructive behavior; impulsive acts; and chronic feelings of emptiness, loneliness, and fear of being abandoned. One-half to two-thirds of individuals who are diagnosed with BPD will also have some type of substance use disorder.
- Because personality disorders share a number of core features, it is not uncommon for individuals diagnosed with BPD to also be diagnosed with other personality disorders.
Treating Individuals with BPD
 BPD is a notoriously difficult psychological/psychiatric disorder to treat. When an individual is diagnosed with BPD and some other comorbid condition, such as a co-occurring substance use disorder or comorbid personality disorder, this makes the treatment process even more complicated. BPD is specifically notoriously difficult to treat because individuals with the disorder will inevitably display:
BPD is a notoriously difficult psychological/psychiatric disorder to treat. When an individual is diagnosed with BPD and some other comorbid condition, such as a co-occurring substance use disorder or comorbid personality disorder, this makes the treatment process even more complicated. BPD is specifically notoriously difficult to treat because individuals with the disorder will inevitably display:
- Noncompliance with treatment: People diagnosed with BPD become very reactive and often demonstrate an extreme resistance to change. This is because individuals with personality disorders often do not see themselves as a problem but instead view everyone else as being the cause of their difficulties. When these individuals have co-occurring substance use disorders, this increases the chances for noncompliance.
- Self-destructive tendencies: BPD patients are often self-destructive and have issues with self-injurious behaviors and suicidality. Because the treatment process attempts to correct dysfunctional behaviors, individuals with BPD must first see the need to change (which means they must accept deficiencies within themselves), which fosters even further issues with self-degradation, suicidality, etc. This often complicates the treatment process.
- Relationship issues: People with BPD have relationship issues with nearly everyone in their lives, and significant relationship issues will often develop with therapists as a result of the therapeutic process of change. The patient may first idolize the therapist and then later totally demonized them (splitting), or may attempt to manipulate different therapists against each other in order to manipulate the overall treatment. Professionals who treat people diagnosed with BPD must be aware of these potentialities and even expect them to occur. Unstable personal relationships within treatment itself as well as outside treatment contribute to the difficulty of helping these individuals adjust.
Despite these issues, there is a very good treatment protocol that is targeted at many of the difficulties these patients exhibit. A specific form of Cognitive Behavioral Therapy known as Dialectical Behavior Therapy (DBT) was originally developed to treat individuals who were suicidal, and the principles were found to be extremely well suited to the treatment of individuals with BPD. As a result, DBT has become the frontline treatment approach for BPD.
The process of DBT includes individual therapy sessions, group therapy sessions, the development of strict rules and regulations that are enforced based on contingencies for not abiding by them, and close supervision and involvement with these patients. The treatment attempts to get individuals to accept certain aspects of reality that are unchangeable and to focus on changing themselves in accordance with their broader needs and goals. As it turns out, DBT is also well suited to treating BPD patients with co-occurring diagnoses (BPD and substance abuse).
Medications can also be used in the treatment of BPD; however, there is no specific medication designed to treat the disorder. Most often, individuals with BPD are put on antidepressant medications, particularly selective serotonin reuptake inhibitors, and other medications that address specific symptoms displayed by the individual. This combination of therapy and medical management can be successful in the long-term management of individuals with BPD and in those who have comorbid disorders.