Benzo Withdrawal Symptoms, Timeline & Detox Treatment
Benzo Withdrawal Symptoms
Benzodiazepines (benzos) are not intended to be taken long-term, as prolonged use or abuse can cause the brain to become both physically and psychologically dependent on them.
Withdrawal symptoms, ranging from a return of uncomfortable psychological symptoms to physical manifestations such as nausea and diarrhea, may occur when the drugs are removed from the bloodstream.
Withdrawal side effects are not generally lethal, although they are best managed with professional medical attention and supervision.
Benzo withdrawal symptoms may include:
- Nausea
- Panic attacks
- Tremors
- Anxiety
- Sweating
- Headaches
- Heart palpitations
- Muscle pain
- Seizures
Benzodiazepines are all designed as central nervous system depressants; however, they each may work slightly differently at targeting certain symptoms. For example, Restoril, Dalmane (flurazepam), and Halcion (triazolam) are considered primarily hypnotic benzodiazepines prescribed for insomnia, while Xanax, Ativan, Librium (chlordiazepoxide), and Valium are classified as anxiolytics used to treat anxiety symptoms. Klonopin is considered primarily an anticonvulsant. Different metabolites of these medications make them slightly different, which may also affect how quickly they leave the bloodstream. Withdrawal from different benzodiazepines is generally thought to bring the same general symptoms; however, it is possible that an individual withdrawing from a hypnotic may have more disrupted sleep patterns while withdrawal from an anxiolytic may include higher levels of anxiety.
Benzodiazepine Withdrawal Timeline
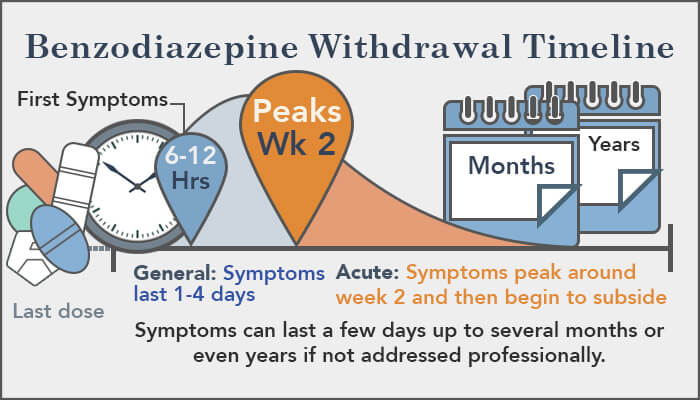
Most benzodiazepine (benzo) withdrawal symptoms start within 24 hours and can last from a few days to several months, depending on the length of the abuse and the strength of the benzo used. Prolonged withdrawal isn’t uncommon, however. About 10 percent of people who abuse benzos still feel withdrawal symptoms years after they have stopped taking the drugs.
Each benzodiazepine medication has a specific half-life that influences the length of time it takes for the drug to leave the bloodstream. If an individual is dependent on a benzo, once the drug is purged from the body, withdrawal may begin. For shorter-acting benzos like Xanax, withdrawal may start within 10-12 hours of stopping the drug. With a longer-acting benzodiazepine such as Valium, it may take a few days for symptoms to appear.
Some short-acting benzodiazepines, like Xanax, are thought to be more potent than some of the longer-acting ones, such as Valium, as well. While withdrawal will be similar for both, users of short-acting benzos may experience withdrawal symptoms sooner and with more intensity, as benzos with longer half-lives will stay in the body longer, therefore slowing the onset of withdrawal.
Benzo Withdrawal Phases

Benzodiazepine withdrawal may occur in three main phases: early withdrawal, acute withdrawal, and protracted withdrawal.
The early withdrawal phase usually starts within a few hours to a few days of stopping the medication and may last a few days. During early withdrawal, an individual may experience a return of anxiety and insomnia symptoms as the brain rebounds without the drugs. Symptoms the benzos worked to suppress may come flooding back. The tapering process frequently used in medical detox may help dampen this rebound effect.
After a few days of stopping a benzodiazepine, acute withdrawal may begin. This phase constitutes the bulk of withdrawal. Symptoms may include anxiety, panic, insomnia, muscle spasms or tension, nausea and/or vomiting, diarrhea, blurred vision, seizures, hallucinations, short-term memory impairment, trouble concentrating, clouded thinking, mood swings, agitation, drug cravings, twitching and weight loss due to a decreased appetite. It is during this phase that specific medications may be most beneficial at targeting some of the certain symptoms. Suicidal thoughts and actions may occur during acute withdrawal from a benzodiazepine as well, and therapy and support groups may help diffuse these complicated emotions. Acute withdrawal may last between two weeks and several months.
Some people, around 10 percent according to a study published by ABC News, may experience protracted withdrawal syndrome that can extend several months or even years after stopping use of a benzodiazepine.
Individuals may experience tingling in their arms and legs, muscle twitches, prolonged anxiety and insomnia, and cognitive deficits as well as depression and mood swings that may be difficult to manage. These symptoms may appear randomly and without warning. Mental health services and support beyond medical detox include therapy and counseling to manage protracted withdrawal symptoms. When a mental health disorder is also present, called co-occurring disorders, specialized treatment that caters to dual diagnoses may be beneficial during recovery.
While there is no hard and fast timeframe for the withdrawal period from a benzodiazepine, medical and mental health professionals can help to greatly reduce the intensity and duration of symptoms that occur during detox. Again, benzo withdrawal should not be attempted without medical supervision. Medical detox can aid in the safe removal of benzodiazepines from the body and brain, and following up with therapy and family support services promotes a smooth recovery.
Benzo Withdrawal Risk Factors
There is no specific timeline dictating exactly how long withdrawal from a benzo, or benzodiazepine, medication will last.
While each individual may experience withdrawal differently, certain estimations can be made. Benzodiazepine withdrawal duration and intensity depend on several factors, including:
- Length of time taking benzodiazepines
- Dosage amount
- Type of drug used/abused
- Method used to take or abuse benzodiazepines
- Underlying medical or mental health issues
- Abuse of other drugs or alcohol concurrently
Family history of drug dependency or previous issues with substance abuse and/or dependency may increase the likelihood of developing a dependency on a benzodiazepine and may potentially add to the withdrawal timeline duration as well.
Benzodiazepines are Schedule IV controlled substances per the Drug Enforcement Administration (DEA). They are sedatives and tranquilizers prescribed to treat symptoms of insomnia, anxiety, panic, seizure disorders, and muscle tensions or spasms. Common benzodiazepines include Xanax (alprazolam), Klonopin (clonazepam), Restoril (temazepam), Ativan (lorazepam), and Valium (diazepam). Alprazolam, the generic name for Xanax, was the 13th most prescribed medication in the country in 2012, according to a survey done by IMS Health.
Individuals taking benzos for several months or more and in high doses are likely to experience more withdrawal symptoms that last longer than those taking smaller doses for a shorter length of time. For example, the U.S. Food and Drug Administration (FDA) reported that patients taking doses of 4 mg/day or higher of Xanax for longer than three months were more likely to become dependent on the drug and therefore more likely to experience more uncomfortable withdrawal symptoms than those taking smaller doses for less time.
The method of ingestion is also related to the onset of withdrawal. For instance, snorting or injecting benzos sends the drugs straight into the bloodstream to take almost instant effect. Ingesting a pill requires that it be digested through the digestive tract, which creates a less intense high and slower onset of withdrawal symptoms.
Take Our Substance Abuse Self-Assessment
Take our free, 5-minute substance abuse self-assessment below if you think you or someone you love might be struggling with substance abuse. The evaluation consists of 11 yes or no questions that are intended to be used as an informational tool to assess the severity and probability of a substance use disorder. The test is free, confidential, and no personal information is needed to receive the result.
