
VA Community Care Network Program Guide and FAQs
What is the VA Community Care Network (CCN)?
The Veterans Affairs Community Care Network (CCN) serves as a vital support system for Veterans requiring healthcare services that the Department of Veterans Affairs (VA) cannot provide. This may happen when Veterans are located in remote areas or have specific healthcare needs that the VA is unable to meet effectively.
The CCN is comprised of a diverse array of healthcare providers, including physicians, clinics, and specialists, who operate within the Veteran’s local community. These external providers often offer a broader spectrum of services compared to the local VA facilities. Notably, they are equipped to treat Veterans facing challenges with substance use disorders, including addiction, as well as those grappling with co-occurring mental health issues.
When Veterans seek care from CCN providers, the services they receive are typically funded or “purchased” by the VA, ensuring that Veterans have access to essential treatments without significant out-of-pocket expenses.
Among these esteemed providers is American Addiction Centers (AAC), recognized as a Community Care Partner. Veterans who require treatment for alcohol or drug misuse can benefit from the high-quality and timely care provided at any AAC facility. This partnership highlights the commitment to ensuring Veterans receive the comprehensive support they need to navigate their recovery and improve their overall well-being.
Contact us to see if you qualify at Or, complete our instant online verification form.
Patient-Centered Community Care (PC3) Regional Networks
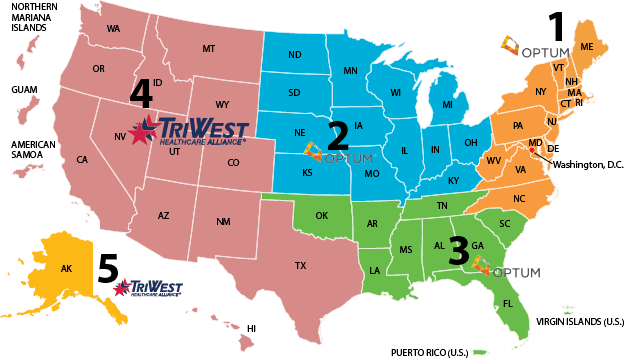
The VA Community Care Network is made up of six regional networks that act as “contract vehicles” for the VA to purchase care for Veterans from local providers when the VA cannot provide appropriate care to a Veteran. These six regional networks act to streamline the process of receiving care for Veterans and beneficiaries.5 (Map Source)
Find Drug & Alcohol Rehab Treatment Near You
How do I find a VA Community Care Network provider?
If you think you’re eligible to receive care at a CCN provider, complete the following steps.
For more information on the process of receiving care with a CCN provider, call the VA.AAC is a Community Care Provider
AAC facilities are part of the VA’s Community Care provider network.
Community Care providers ensure that Veterans receive timely and high-quality care. To obtain certification as a Community Care provider, a treatment provider must enter into a Veterans Care Agreement with the VA and meet its stringent criteria.1
Veterans seeking treatment can rest assured that AAC has met all of the VA’s certification guidelines. In addition, providers such as AAC can access the VA’s improved technology systems, which allow for electronic file sharing to expedite the referral and treatment process.1 Providers are also able to access required training materials from the VA, which helps to maintain high standards of care.1
AAC’s Program for Veterans
AAC’s Veteran program is specially designed to treat first responders and Veterans with substance use and mental health disorders, such as depression, post-traumatic stress disorder (PTSD), and anxiety.
AAC is the leading provider of addiction treatment in the U.S. We specialize in evidence-based treatment and believe in providing treatment that addresses addiction from every angle. This means that AAC’s treatment methods have been thoroughly evaluated and proven effective in scientific research. In addition, all treatment programs are tailored to meet your specific needs.
AAC is the leading provider of addiction treatment in the U.S. We specialize in evidence-based treatment and believe in providing treatment that addresses addiction from every angle. This means that AAC’s treatment methods have been thoroughly evaluated and proven effective in scientific research. In addition, all treatment programs are tailored to meet your specific needs.