Finding an Eating Disorder Treatment Center Near Me
Eating disorders are serious mental health disorders with severe and life threatening medical and psychological consequences if untreated. They are not issues of willpower or methods of dieting but potentially deadly diseases that require professional medical and therapeutic treatment and support.
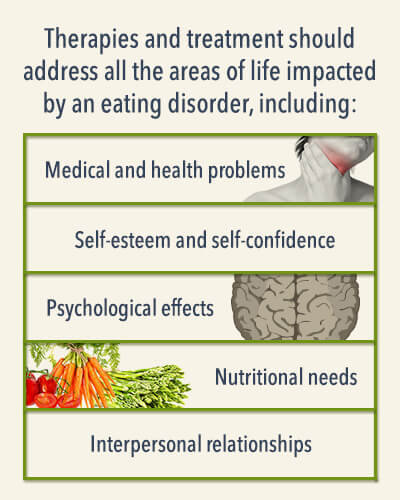
An eating disorder treatment center should offer clients everything necessary to manage the symptoms experienced due to the eating disorder as well as any and all co-occurring disorders (e.g., substance abuse, depression, anxiety, medical disorders, etc.). Treatment should offer clients access to everything they need to find stability and manage their symptoms. To that end, therapies and treatment should address all the areas of life impacted by an eating disorder, including:
- Medical and health problems
- Nutritional needs
- Self-esteem and self-confidence
- Interpersonal relationships
- Psychological effects
Clients are encouraged to seek an eating disorder treatment program that is well-rounded in nature at the earliest signs of a disorder. Without treatment, eating disorders can be fatal. They can lead to a range of chronic and acute disorders that diminish quality of life and that can be life-threatening in some cases. Therapy, support from peers and staff, family support, and in some cases, certain medications can all contribute to the client’s ability to function without resorting to disordered eating habits, to get to and maintain a healthy weight, and to create a new life in recovery.
Is It an Eating Disorder?
The signs and symptoms of an eating disorder will vary according to the specific disorder and the individual experiencing the symptoms. In general, however, those who are struggling with an eating disorder often:
- Struggle with maintaining a healthy weight
- Talk about dieting and calorie management
- Believe they are fat
- Struggle with low self-esteem and warped self-image
- Struggle with co-occurring disorders, including depression, anxiety, and/or substance abuse
Anorexia
Anorexia nervosa has been identified as the most lethal mental health disorder. It is defined by a fear of weight gain, and those who struggle with the disorder may believe they are fat when they are underweight, exhibit an extreme distaste for anyone who is overweight, and significantly limit their caloric intake to the point of starvation. Extreme limitation of calories can quickly result in malnutrition, chronic fatigue, mood swings, and the failure of organs that depend upon certain nutrients to function. If untreated, the disorder can be deadly; in fact, people living with the disorder have a six-fold increased chance of death over the general population.
Signs and symptoms of anorexia may include:
- Extreme weight loss or maintaining an extremely low weight
- Distorted body image
- Taking over-the-counter or prescription medication with the goal of curbing appetite, increasing metabolism, and/or increasing urine output or bowel movements
- Eating very little or pushing food around the plate without actually eating
- Refusing to eat in public or in front of people
- Practicing extreme rituals and placing limitations on eating (e.g., eating only organic or gluten-free foods, avoiding whole food groups, eating only at certain times or eating foods in a certain order, etc.)
- Obsessively weighing food before eating and/or counting and calculating calories
- Going to extreme measures to burn calories, including vomiting or exercising to exhaustion or when sick or injured
- Being extremely judgmental of those who are overweight
- Obsessively talking about dieting, calories, or weight loss
- Struggling with mood swings, moodiness, and/or personality changes
Bulimia
Bulimia nervosa is a disorder characterized by binge eating followed by feelings of a loss of control and an attempt to regain that control through quickly ridding the body of the unwanted calories. People living with bulimia may attempt to purge calories and prevent weight gain caused by binge eating through such means as self-induced vomiting, use of laxatives, excessive exercise, or a combination of behaviors.
Bulimia is cyclical pattern of behavior. Some people living with the disorder may binge and purge daily while others may only do so a few times each week. Additionally, some people live with both anorexia and bulimia. They significantly limit their intake of calories for a period of time then take part in a binge session, eating a large amount of food, and then take measures to attempt to stop the absorption of those calories. Unlike people living with only anorexia, however, those struggling with bulimia may be at a normal weight for their height, underweight, or overweight.
Signs of bulimia include:
- Binge eating sessions where a large amount of food is consumed at once, often in private
- Self-induced vomiting to purge unwanted calories ingested during the binge eating session
- Use of laxatives, water pills, and/or enemas in an attempt to purge calories before they are absorbed
- Compulsive exercise in an attempt to burn as many or more calories than ingested
- Purchasing large amounts of food that disappear inexplicably
- Routinely going to the bathroom right after eating, especially after eating a lot of food
- Swollen face and puffy eyes and/or broken eye blood vessels
Additionally, people living with bulimia may have damaged tooth enamel, swollen glands, an inflamed throat, and reflux and/or dehydration.
Binge Eating
Binge eating disorder (BED) is the most commonly diagnosed eating disorder in the country and is defined by eating large quantities of food ” as much as 5,000-15,000 calories ” in a single sitting, then experiencing feelings of guilt and shame as a result. Binge sessions may occur after a period of stringent caloric restriction or dieting ,and they are often characterized by feelings of a loss of control.

Those who struggle with binge eating are often overweight or obese and, as a result, are likely to struggle with medical problems such as heart disease, some cancers, high blood pressure, gallbladder disease, high levels of “bad” cholesterol, and/or type II diabetes.
Some signs and symptoms of binge eating disorder include:
- Overeating throughout the day, snacking often, and/or eating large amount of food in one sitting after a period of minimal food intake
- Compulsive engagement in binge eating sessions
- Eating very quickly
- Eating beyond fullness to the point of discomfort
- Eating when bored, depressed, or experiencing other uncomfortable emotions
- Eating when not hungry
- Engaging in binge eating in private
- Experiencing feelings of self-loathing, disgust, shame, or remorse after a binge eating session
People who struggle with binge eating may also be living with another eating disorder or display other disordered eating habits.
Eating Disorder Not Otherwise Specified (EDNOS)/Other Specified Feeding or Eating Disorder (OSFED)
When a person’s unique combination of disordered eating habits does not add up to bulimia or anorexia, the diagnosis was “Eating Disorder Not Otherwise Specified”(EDNOS) until the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) was updated. Currently, EDNOS is not a valid diagnosis. Rather, the term “Other Specified Feeding or Eating Disorder”(OSFED) is used to diagnose those who are living with a feeding or eating disorder that is intrusive in their lives emotionally and/or physically, causing distress or impairment, but does not fit the diagnostic criteria of anorexia or bulimia. In some cases, the person’s experience may be similar in nature to that of someone living with anorexia or bulimia but vary just enough to be outside the diagnostic parameters for those disorders.
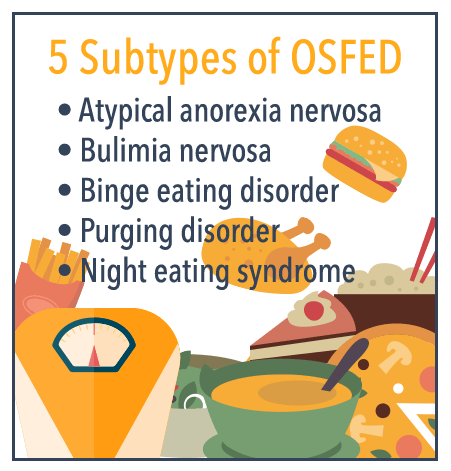
According to the National Association of Anorexia Nervosa and Associated Disorders (ANAD), there are five subtypes of OSFED. These include:
- Atypical anorexia nervosa: Those who meet all the criteria for anorexia but who are maintaining a normal weight are diagnosed with OSFED.
- Bulimia nervosa: Those who purge regularly after eating but engage in the practice less frequently than twice a week, or who have been purging three or more times a week for less than three months will be diagnosed with OSFED rather than bulimia.
- Binge eating disorder: People who engage in binge eating sessions, ingesting large amounts of food but who not do not feel out of control during or after the experience may be diagnosed with OSFED.
- Purging disorder: Those who do not binge before purging (e.g., using laxatives or enemas inappropriately or inducing vomiting) may find that their diagnosis falls into this category.
- Night eating syndrome: Eating after waking in the middle of the night or eating large amounts of food before bed are characteristic of this diagnosis.
Additionally, other disordered eating behaviors that have been reported by patients seeking treatment that may be classified as an OSFED include exercise addiction (counting calories and obsessively exercising to ensure that more calories are burned than ingested to the point of exhaustion and despite illness or injury) and orthorexia (an unhealthy commitment to “healthy” eating that ultimately overly restricts intake of necessary nutrients or calories), among others.
Finding the Right Treatment for Your Needs

Treatment for an eating disorder of any nature should focus on the specific triggers that a person faces and incorporate a range of therapeutic options and interventions, including any combination of the following:
- Personal therapy
- Family therapy
- Support groups
- Nutritional counseling
- Fitness programs
- Medications, if necessary
What Are the Best Options for Treating Bulimia and Anorexia?
The American Psychological Association (APA) supports a range of therapeutic treatment options for people who are living with bulimia and/or anorexia. Because the driving forces behind these disorders (e.g., poor body image, low self-esteem, depression, anxiety, and peer pressure) are often just as important as the manifestation of the disorder in terms of the direction of treatment, the focus of therapies for both conditions may be similar though the structure may be different.
Anorexia
In past years, treatment professionals have removed family from the equation when helping someone to learn how to manage anorexic behaviors, especially in the case of young people and their parents. In many cases, parental influence and expectations play a role in the young person’s development of anorexia, thus it was thought that by removing that influence the person in treatment would have a greater chance at making progress in recovery.
Today, however, most treatment options emphasize family support and recognize it to be one of the most important factors in a person’s ability to learn how to manage eating behaviors. One research-based, short-term treatment for anorexia is called the Maudsley approach. Essentially a family-based treatment, family members, the person living with anorexia, and therapists all get together for a picnic meal in one of the early sessions. The goal is to educate therapists on eating habits and rituals in the family and family members’ attitudes toward eating while giving therapists the opportunity to help family members better understand how they can empower their loved one to eat more healthfully.
In following sessions, family members have the chance to discuss what they have tried in the past in terms of helping their loved one to engage in healthy eating behaviors at mealtime ” what has worked and what hasn’t. This treatment approach also empowers the person’s sense of independence in self-management of eating while learning how to manage stressors in life that may contribute to the urge to limit caloric intake.
Bulimia
Two types of psychotherapy are research-based and demonstrated to be effective in the treatment of bulimia: Cognitive Behavioral Therapy (CBT) and interpersonal therapy. Cognitive Behavioral Therapy assists the person in recovery in identifying all the unrealistic and negative self-expectations that may be triggering the urge to binge and then purge. Once identified, people in recovery can begin to make changes in their lives that will make it easier to avoid bingeing and purging.
Interpersonal therapy assists people in recovery in working on the quality of their relationships with other people. With a shift toward more realistic expectations of what a relationship can and should be and improved communication skills, it may be possible to have stronger relationships that are less stressful, which in turn make it easier to avoid engaging in disordered eating habits.
Where Can People Go for Binge Eating Treatment?
Like treatment for anorexia and bulimia, treatment for binge eating disorder should include a range of treatment options. Goals for BED recovery will vary based on the needs and desires of the client, but may include:
- Cutting back on the frequency of binge eating sessions each week or month
- Increasing the number of healthy eating choices
- Increasing the number of exercise sessions
- Addressing feelings of remorse, guilt, or shame caused by binge eating
- Improving body image, self-acceptance, and self-esteem
- Embarking on treatment that addresses co-occurring mental health symptoms (e.g., depression, anxiety, grief, trauma, abuse, etc.)
- Getting medical care for any ailment caused or exacerbated by binge eating
Both inpatient and outpatient treatment options may be appropriate for the treatment of BED. Prospective clients are encouraged to talk to potential treatment centers in advance to learn more about the specific treatment options provided by each program and to determine which style and type of treatment will best suit their needs.
Statistics and Facts
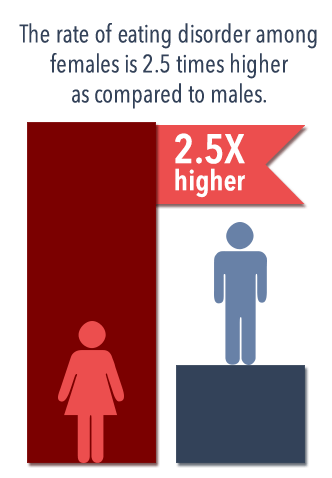
- People of all genders and ages may struggle with eating disorders, however, the rate of eating disorders among females is 2.5 times higher as compared to males.
- The first signs of an eating disorder are most likely to appear during the teen years or early adulthood but could begin at any time including during childhood, midlife, or older adulthood.
- There are a number of issues that can potentially contribute to the development of an eating disorder. Some combination of the following may be potential causes of disordered eating habits:
- Feelings of low self-esteem or self-worth
- Cultural expectations to remain thin, trim, and often underweight
- Co-occurring mental health disorders like mood disorders or personality disorders
- Acute, stressful life events that are life-threatening or result in extreme, unwanted change (e.g., loss of a loved one, divorce, job loss, etc.)
- Hormone and brain chemical levels and balances
- Family expectations and pressures
Anorexia:
- According to a report published in the journal JAMA Psychiatry that analyzed 36 different studies on mortality rates and eating disorders, it was discovered that, each year, the United States loses 5.1 people per 1,000 people living with anorexia, 1.7 people per 1,000 people living with bulimia, and 3.3 people per 1,000 patients diagnosed with EDNOS. Additionally, one in five deaths caused by anorexia were suicides.
- Though anorexia can occur in anyone, an estimated 85-90 percent of people living with the disorder are female.
- Though some people who have been living with anorexia and its physical effects for years may require inpatient care initially in order to stabilize early in treatment, outpatient care may be intensive enough to help up to two-thirds of patients to recover from anorexia and learn how to eat healthfully.
- Personal therapy, especially Cognitive Behavioral Therapy, has proven to be effective in the treatment of anorexia, but family-based therapies have also been demonstrated to play a critical role in helping someone to stabilize in recovery, according to a study published in the Archives of General Psychiatry.
Bulimia:
- Though bulimia can occur in all populations, the disorder most commonly occurs in young white females: an estimated 1-2 percent of American girls are living with bulimia nervosa. An estimated 85-90 percent of people diagnosed with the disorder are female.

- About 75 percent of patients living with the disorder begin to exhibit symptoms before the age of 22, most frequently around the age of 15 or 16.
- Purging, the behavior that separates bulimia from binge eating, can occur in a number of different ways and doesn’t not always necessarily indicate self-induced vomiting. Over-use of laxatives, enemas, diuretic pills, and exercise to attempt to rid oneself of unwanted calories are all behaviors that may qualify someone for a bulimia diagnosis.
Binge Eating:
- An estimated two-thirds of people living with binge eating disorder are obese.
- Binge eating contributes to the development of obesity, which in turn can trigger a host of chronic health disorders, according to the US Department of Health and Human Services (HHS).
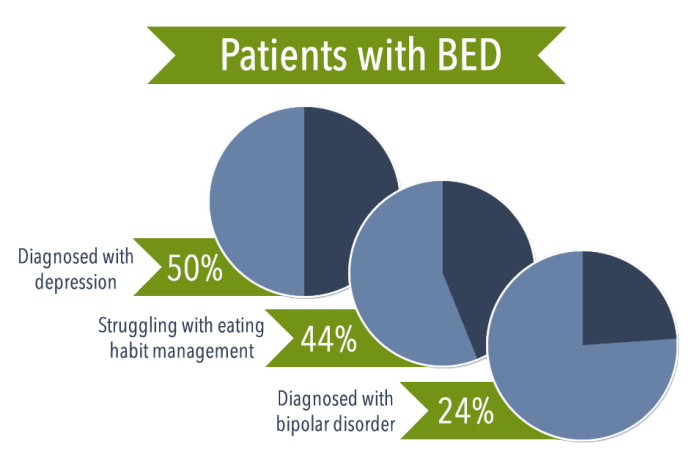
- Binge eating disorder is the most commonly diagnosed eating disorder, and an estimated 3 percent of Americans are living with the problem. Additionally, about 50 percent of patients with BED are also diagnosed with depression, 24 percent are diagnosed with bipolar disorder, and 44 percent self-report struggling with eating habit management.
- Cortisol released during the stress response and the corresponding storage of fat in the abdominal area are increased issues for those living with BED and obesity as compared to the general public, according to a study published in the journal Appetite. Stress can also be a trigger for binge eating.
- Binge eating has been linked to increased rates of suicidal thoughts and behaviors, especially if the person with BED struggles with feelings of low self-worth and/or feels lacking.
- People living with binge eating disorder very often also struggle with disrupted sleep patterns, including difficulty falling asleep, waking at night to eat, and struggling to go back to sleep.
- The National Institute of Diabetes and Digestive and Kidney Diseases reports that people living with binge eating disorder are at higher risk of developing such health problems as headaches, joint and muscle pain, sleep apnea, digestive problems, high blood pressure, osteoarthritis, kidney disease, heart disease, stroke, diabetes, certain cancers, and fatty liver disease. They also experience difficulty in getting or maintaining a healthy pregnancy.

