Depression & Substance Abuse
Although the user may rely on substances used to relieve symptoms of depression, chemical intoxication can actually make depressive episodes more severe, increasing the frequency and intensity of negative thoughts and self-destructive behavior.
A rehab program that addresses both depression and addiction may help to stop the progression of both disorders and empower the individual to build a healthy, sober life in recovery.
Learn how American Addiction Centers may be able to help get you through depression and substance abuse issues at the same time by calling our toll-free and confidential national addiction hotline at .
Common Symptoms of Depression
Unlike ordinary sadness or grief, which can occur temporarily after a loss, the symptoms of depression occur nearly every day for weeks—sometimes months or years—interfering with all aspects of an individual’s life.
To meet the diagnostic criteria for depression established by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), a person must experience 5 or more symptoms of the disorder almost every day for at least 2 weeks, and these symptoms must not be related to a coexisting medical condition or the effects of substance abuse.2 They include:2
- A low, depressed mood.
- A loss of pleasure or interest in daily activities.
- Persistent feelings of self-hatred, worthlessness, or guilt.
- Sleep disturbances, such as sleeping too much or too little.
- Unintentional weight loss or gain.
- Physical fatigue.
- Low energy levels, with slower than usual responses and movements.
- Problems with concentration or memory.
- Persistent, intrusive thoughts about death or dying.
- Suicidal thoughts or suicide attempts.
The symptoms of depression can cause noticeable problems with work, school, family life, and social relationships. People experiencing a depressive episode may have trouble getting out of bed in the morning due to a lack of energy, fatigue, and a loss of motivation.
They may lose interest in hobbies or pursuits that they were once passionate about or avoid activities that used to give them pleasure. They may be frequently tearful, talk about harming themselves, or become obsessed with thoughts and images of death.
For the loved ones of a depressed person, dealing with the symptoms can be both frightening and frustrating. It’s normal to try to cheer up a friend or to encourage them to “snap out of it”; however, depressive symptoms do not respond to these offers of help.
Understanding Depression
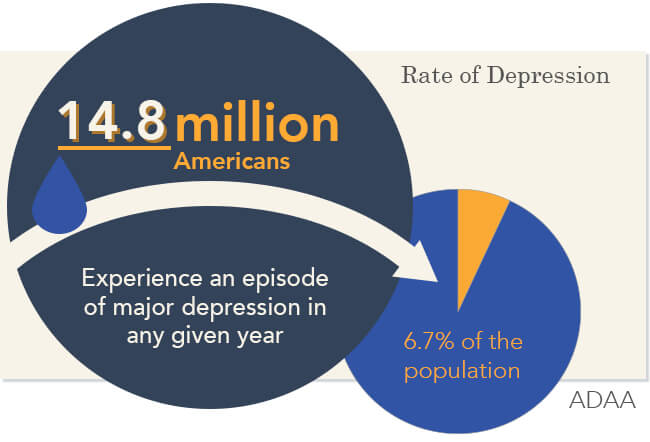
Over 350 million people suffer from depression worldwide, and only about 50% of these individuals will ever receive treatment.3 In the United States, over 15 million adults experience an episode of clinical depression in any given year—close to 7% of the population.4
Depression can have an impact on physical and emotional wellbeing, as well as personal relationships, occupational status, and financial health. But how does depression differ from a long case of the blues?
A mood disorder like depression is not the result of bereavement or a personal setback, such as the death of a loved one or loss of a job, but a chronic, progressive illness that may get worse without treatment.
The only way to treat this serious disorder effectively is through professional therapeutic interventions, such as behavioral modification, support groups, motivational therapy, and antidepressant medications.
Types of Depressive Disorders
Depression can take several different forms based on the severity, duration, and cause of its symptoms. Depression may be best understood as a spectrum of moods rather than a series of separate, clearly defined categories.5
For the sake of diagnosing and treating this serious disorder, psychiatric experts have identified several categories. Along with these categories, there are a number of depressive disorders associated with specific life stressors, psychological conditions, or emotionally taxing situations. These situational disorders share many of the symptoms of general depression, but they occur under specific circumstances and may resolve once these situations are changed.
Depression & Substance Abuse

Research has revealed that many of the factors that contribute to depression also play a part in substance use disorders. This is known as co-occurring disorders, or a dual diagnosis. Depression and addiction frequently involve:
- Imbalances in brain chemistry.
- Family history.
- Past trauma.
In addition, the physical and psychological effects of addiction may mask the signs of depression or worsen the symptoms of this psychiatric illness.
Connection Between Alcoholism & Major Depression
There’s a strong connection between alcoholism and major depression.9
In a nationwide study of 43,093 adults 18 years old and over, researchers found that for those suffering from a current alcohol addiction, there was evidence that over 20% of them also met the criteria for that of a comorbid major depressive disorder.9
Survey respondents in search of treatment for an alcohol use disorder were over 40% more likely than the general population to have at least one mood disorder.9
Alcohol is a central nervous system depressant that may initially function as a stimulant, but that quickly intensifies feelings of lethargy, drowsiness, and depression. Alcohol use, which lowers inhibitions and impairs judgment, can also increase the risk that a depressed individual will attempt suicide.10
Alcohol and drug abuse can worsen the course of a depressive disorder by aggravating the symptoms of depression, increasing the likelihood of hospitalization, and interfering with the course of treatment. Individuals who are being treated for depression while using drugs or alcohol are unlikely to see positive outcomes from therapy unless the substance abuse is taken into account and treated concurrently.
Substance abuse can impair motivation and decreases the effectiveness of therapeutic interventions. In addition, alcohol or drugs can have dangerous interactions with the medications used to treat depression.
The most effective approach to treating depression is a program that integrates mental health and recovery services at the same facility, with a staff of professionals who are cross trained in both fields.
Investigating the Causes of Depression
Depression is one of the most common and most debilitating mood disorders, yet researchers still haven’t determined the exact cause of this condition. There are, however, several theories about the roots of depression.
Brain Structure
The brains of some individuals with depressive disorder are structurally different from those who do not have depression. MRI imaging studies reveal that the areas of the brain that are responsible for mood, cognition, metabolic function, and sleeping have a unique appearance in people who have serious mood disorders.11
Environment & Childhood Experience
A disorderly home environment or a history of physical, sexual, or emotional abuse in childhood can increase the chances of developing depression in adolescence or adulthood.12 Trauma therapy can be extremely useful for processing unresolved memories and healing the suppressed emotional wounds that can contribute to depression later in life.
Genetics
The neurological differences that distinguish people with depression are at least partly hereditary. Genetic research shows that people who have a close relative, such as a parent or sibling, with depression are 20 to 30% more likely to suffer from depression themselves.13
Unlike diseases that are linked to a specific, defective gene, such as cystic fibrosis, depression is more likely to be linked to several genes.
Situational Factors
Although the losses that we all experience do not necessarily cause depression, a severe setback can trigger a depressive episode. For instance, the death of a loved one or a bitter divorce could send a person into a period of grief and bereavement, which may turn into depression if the emotions surrounding that loss are not adequately resolved.
Unlike bereavement, depression is often accompanied by feelings of worthlessness, self-loathing, or suicidal thoughts.
Brain Chemistry
Neurologists and pharmacologists have long pursued the connection between brain chemistry and depression in an effort to offer solutions to this disabling condition. Depression has been linked to imbalances in the brain chemicals, or neurotransmitters, that regulate emotional states, moods, energy levels, and appetite, such as serotonin, norepinephrine, and dopamine.14
As with other types of chronic mental illness, there are usually several factors involved in the development of depression. A family history of depression, for example, may be combined with a history of past trauma or the breakup of a marriage to make an individual more vulnerable to depression.
Getting Help for Depression & Co-Occurring Addiction
Living with a family member or spouse who is in a depressive episode can be both painful and stressful. It’s natural for loved ones to feel helpless, frustrated, and even emotionally drained by their experiences dealing with depression. Approaching a relative or friend about depression and substance abuse is very hard, but it can also prevent serious harm to the individual.
Without help, it’s likely that the addictive disorder and the depression—both chronic illnesses—will continue to get worse until the individual becomes severely ill. It’s even possible that an intervention by loved ones may help to prevent a suicide attempt and save the individual’s life.
People struggling with depression often feel isolated, profoundly lonely, and powerless. Offering support and practical solutions could make an enormous difference in the way a depressed person feels about the future.
Mental health professionals can be valuable partners in the process of intervening on behalf of someone who has depression. With the guidance of a therapist, families can learn about the facts behind depression and develop a better understanding of how to relate to someone who has this disorder.
If substance abuse is a factor, a therapist or intervention specialist can provide guidelines on how to effectively get help for someone with depression.
Therapies & Interventions
The treatment of depressive disorders with co-occurring addiction can be challenging. Depressive symptoms such as low motivation, low self-worth, and a flat emotional affect may imitate the effects of chemical intoxication or withdrawal.
In order for the treatment team to distinguish between the effects of depression and substance abuse, the client must undergo a thorough psychiatric assessment.15 Although major depressive disorder is one of the most serious, debilitating types of mental illness, it’s also very treatable with the right combination of therapeutic strategies. With the help of qualified, licensed mental health professionals, depressed individuals can be treated, and their families can recover hope for the future.16

Medications for Depression
The most widely prescribed medications for depression are drugs in the SSRI category, such as:
- Fluoxetine (Prozac).17
- Citalopram (Celexa).18
- Sertraline (Zoloft).19
These drugs correct chemical imbalances by increasing the level of serotonin, a neurotransmitter that affects mood, to the brain. SSRIs are now considered to be frontline pharmaceutical treatment for depression, as they have relatively mild side effects compared to older antidepressant medications.
Cognitive Behavioral Therapy (CBT)
CBT addresses the dysfunctional thoughts and actions that affect people with mood disorders like depression.20 Rather than delving into the roots of depression, CBT focuses on identifying and transforming self-defeating ideas and repetitive self-talk, such as “I’m worthless,” “I’ll never feel better,” or “I might as well drink, my life is so bad.”
Such negative thoughts can be replaced by more positive messages, while maladaptive coping skills can be replaced with more effective approaches to life’s stressors and triggers.
Motivational Interviewing (MI)
Unlike older, confrontational approaches to rehab and recovery, MI takes a positive, encouraging perspective, engaging the client in the recovery process through an active collaboration with the therapist.21
MI, as a therapeutic strategy, can be highly effective for individuals with depression, who have difficulty finding and maintaining internal sources of motivation. 21
Trauma Therapies
If a history of trauma is a factor in a client’s depression or substance abuse, trauma therapies like Seeking Safety and eye movement desensitization reprocessing (EMDR) can help. These therapies help to reprocess troubling memories and resolve old sources of emotional pain, so the client can move on through the process of recovery and rehab.
Family Systems Therapy
Family systems therapy treats the client’s household unit as a whole, and the diseases of depression and addiction as family problems rather than individual disorders. Therapeutic goals for families include:
- Educating loved ones about depression and addiction.
- Improving communication among family members.
- Setting realistic boundaries.
- Establishing an environment at home that supports sobriety.
Treating Co-occurring Depression & Substance Abuse

When substance abuse occurs with a depressive disorder, treatment should focus on both disorders at the same time. Treatment plans should be developed that take the client’s depressive symptoms—such as low motivation, low energy levels, and feelings of hopelessness—into account, while addressing the addictive behavior.
In the initial stages of recovery, inpatient treatment at a residential recovery facility may be recommended, especially if the individual expresses suicidal thoughts or has a history of suicide attempts.
In an inpatient setting, clients can go through detox and rehab with the 24-hour support and supervision of a staff of clinicians and therapists. Once the client is ready to progress to the next stage of recovery, a partial hospitalization program or outpatient program will offer a higher level of independence and self-determination.
Clients should be monitored closely at every stage of rehab to ensure that their level of treatment is appropriate for their current psychological status.
Throughout substance abuse treatment, core interventions such as individual therapy, group therapy, 12-Step programming, and family or marriage counseling provide a stable support network and a foundation for psychological healing.
Starting the Path to Recovery
Depression can have devastating effects on an individual’s wellbeing and on the lives of loved ones. Fortunately, the feelings of sadness, worthlessness, and despair that mark depression can be greatly reduced through research-based therapies.
Many clinically depressed individuals have also shown considerable improvement in their symptoms through pharmacotherapy. To maximize the outcomes of treatment, clients should have a range of resources available that address their psychological, medical, and psychosocial needs.
Statistics confirm that alcohol addiction and drug addiction are more common among people with depression than in the population as a whole. Individuals with both mental illness and substance abuse disorders require integrated treatment plans that encompass their mental health needs as well as their need for detox and rehabilitation.

