Alcohol and Drug Abuse Statistics (Facts About Addiction)
How Many Americans are Addicted to Drugs or Alcohol?
According to the 2024 United States National Survey on Drug Use and Health (NSDUH):
- 48.4 million (16.8%) Americans aged 12 and older battled a substance use disorder in 2024.1
- 27.9 million Americans 12 and older had an alcohol use disorder in 2024.1
- Meanwhile, 28.2 million Americans 12 or older reported battling a drug use disorder in the past year.1
- 1 in 6 (7.7 million) of these people who suffered from SUD in the past year struggled with both alcohol and drug use disorders simultaneously.1
- In 2024, 21.2 million adults suffered from both a mental health disorder and a substance use disorder.1
Understanding the National Scope of Addiction
These figures aren’t just numbers. They represent millions of Americans and families impacted by addiction every year. When 1 in 6 people with SUD struggle with both alcohol and drug addiction, and over 21 million adults are navigating co-occurring mental health and substance challenges,1 it highlights a critical public health concern.
Understanding how many Americans struggle with addiction inform better policy, increase access to treatment, and reduce stigma. Most importantly, it reminds those affected that they’re not alone, and that help is available.
Causes of Addiction
- Genetics, including the impact of one’s environment on gene expression, account for about 40% to 60% of a person’s risk of addiction.2
- Environmental factors that may increase a person’s risk of addiction include a chaotic home environment and use, parental drug use and attitude toward ’ drugs, peer influences, community attitudes toward drugs, and poor academic achievement.2
- Teenagers and people with mental health disorders are more at risk for drug use and addiction than other populations.2
Drug and alcohol use can be scary. What’s more frightening is when you’re the one battling a substance use disorder (SUD) or an alcohol use disorder (AUD), and you don’t have a solution to the problem.
American Addiction Centers (AAC) provides 24-hour medical detox, premium rehabilitation treatment, and ongoing care. If you’re struggling with an AUD or SUD and are looking for a solution, reach out to one of our admissions navigators.
Substance Use Disorder Statistics for Specific Population Demographics<
Rates of substance use, addiction, and related issues vary by age, gender, ethnicity, and other demographic classifications.
Addiction Can Affect Anyone
It’s important to note that substance use disorder doesn’t discriminate. People from all walks of life — regardless of age, gender, cultural background, or socioeconomic status — can experience addiction.
Whether you’re a student, parent, Veteran, professional, or retiree, substance use challenges may affect you. What matters most is not where you’ve come from, but the support you seek moving forward. Recovery is possible, and getting the help you need is the first and most important step toward reclaiming your health and future.
Statistics on Addiction to Specific Substances
Now, let’s take a look at addiction and misuse of specific substances.
Alcohol
- In 2023, an estimated 28.9 million Americans aged 12 and older battled an alcohol use disorder, or 10.2% of this population.1
- Over half of all American adults have a family history of problem drinking or alcohol addiction.9
- Around 10.5% of U.S. children (75 million) live with a parent with alcohol use disorder, based on a 2017 report by SAMHSA.10
- An estimated 88,000 people die from alcohol-related causes annually.9
- Alcohol is the 5th-leading cause of preventable death in the United States.11
Cocaine
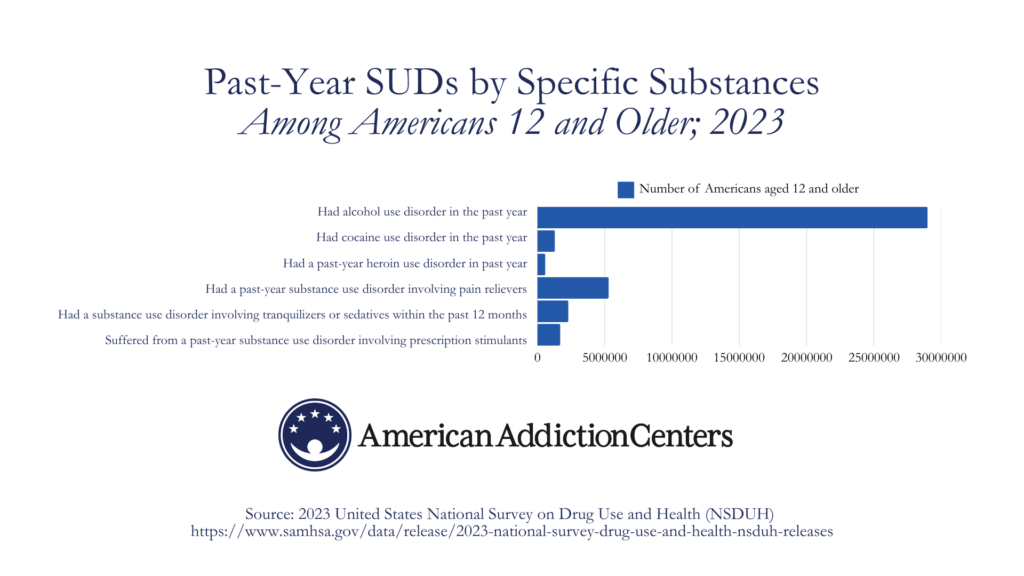
According to the 2023 NSDUH:
- About 1.3 million Americans 12 years old or older (0.4%) struggled with a cocaine use disorder in the past year.1
- 298,000 people aged 12 and older received inpatient treatment for a cocaine use disorder in the past year.1 542,000 received outpatient treatment.
Heroin
- About 587,000 people age 12 and older (0.2%) had a past-year heroin use disorder in 2023.1
- Around 23% of people who use heroin will become addicted to it.5
- Based on 2021 data, the yearly number of heroin overdose deaths have tripled since 2010.13
- Around 372,000 people surveyed in 2023 received inpatient treatment for heroin use disorder in the past year. 832,000 received outpatient treatment.
Prescription drugs
According to the 2023 NSDUH:
- The most common types of prescription drugs misused in the past year were pain relievers, tranquilizers, stimulants, and sedatives.1
- Around 5.3 million people age 12 and older had a past-year substance use disorder involving pain relievers, or about 1.9% of this population.1
- 2.3 million Americans aged 12 or older (0.8%) had a substance use disorder involving tranquilizers or sedatives within the past 12 months.1
- 1.7 million of Americans 12 or older (0.6%) suffered from a past-year substance use disorder involving prescription stimulants (e.g., Adderall, Ritalin).1
Marijuana
According to the 2023 NSDUH:
- 19.2 million (6.8%) Americans aged 12 or older battled a marijuana use disorder in the past year.1
- 43.6 million Americans (15.4%) aged 12 or older surveyed used marijuana in the past month.
- 479,000 Americans 12 or older received inpatient treatment for marijuana addiction in the past 12 months. 1.7 million received treatment at an outpatient center.1
Statistics on Addiction Treatment
- In 2024, an estimated 18.2% of people aged 12 and older (52.6 million people) needed treatment for a substance use disorder in the past year. Only 23% of those received the treatment needed.1
- In 2024, 93.3% of the 1.7 million adolescents aged 12 to 17 with a substance use disorder did not receive treatment and did not think they needed it.1
- In 2024, 45.3% of Americans 18 or older who could not get the treatment they needed in the past year said they did not seek treatment because they thought it would be too expensive. 59.5% said they were not ready to cut back or stop using alcohol or drugs, and 38.9% said they didn’t know where to go or how to get treatment (respondents could cite multiple reasons).1
- Alcoholics Anonymous (AA) has more than 120,000 groups in more than 175 countries around the world, with almost 2 million members.14
- The relapse rate for substance use disorders is estimated to be between 40% and 60%. This rate is comparable to rates of relapse for other chronic diseases such as hypertension or asthma.15
- According to the 2023 NSDUH, 2.3 million Americans 12 years old or older (0.8%) underwent addiction treatment that utilized medications for opioid use disorder (MOUD) in the past year.3
- In 2023, around 4.5 million Americans 12 or older (1.6%) received treatment for alcohol use disorder in the past year.
Why These Treatment Statistics Matter
The gap between those who need treatment and those who receive it is staggering and deeply concerning. With over 54 million Americans in need of addiction treatment and only 23% receiving it,1 millions continue to suffer without support. These aren’t just numbers; they represent lives at risk, families in crisis, and communities affected by untreated substance use.
This reinforces the importance of education, early intervention, and accessible care.
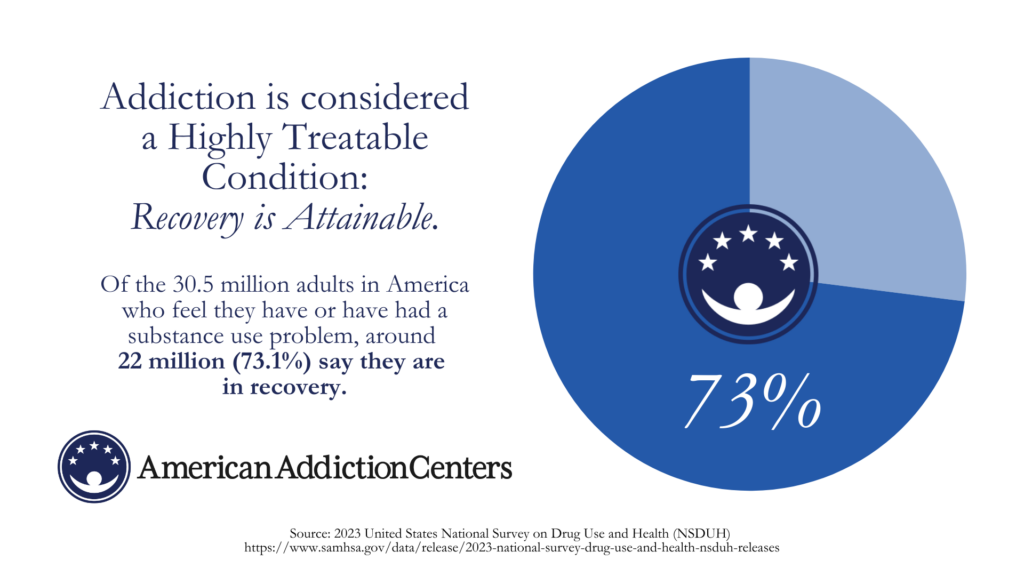
Financial concerns, stigma, and a lack of information are major barriers preventing people from seeking help. That said, addiction is considered a highly treatable condition, and recovery is attainable. Of the 30.5 million adults in America who feel they have or have had a substance use problem, around 22 million (73.1%) say they are in recovery.3
Find Addiction Treatment That Works for You
American Addiction Centers (AAC) operates several facilities across the U.S., providing multiple levels of care and specialized treatment tracks for specific demographics, such as Veterans, LGBTQ+, and more.
Speak to a compassionate admissions navigator, learn more, and begin treatment today. You can also verify your insurance online by using the confidential form.