Suboxone Withdrawal: Symptoms, Timeline & Detox Treatment
What Is Suboxone Withdrawal?
Suboxone is a prescription drug that is used as part of an opioid treatment program that includes behavioral therapy and counseling. Suboxone, which contains buprenorphine and naloxone, can be an effective medication for opiate dependence and is often taken for long periods of time after the user has stopped using addictive opioids. Despite its effectiveness, Suboxone can also be addictive and produces similar withdrawal effects to other opioids if quit suddenly.
Individuals should avoid abruptly discontinuing regular use of Suboxone and seek the care of a doctor or other treatment professional to receive a supervised schedule of discontinuation to mitigate the risks of an overtly unpleasant withdrawal.1
The withdrawal symptoms of Suboxone can vary in severity and duration, depending on how long the individual has been taking Suboxone, as well as the dosage of the drug.
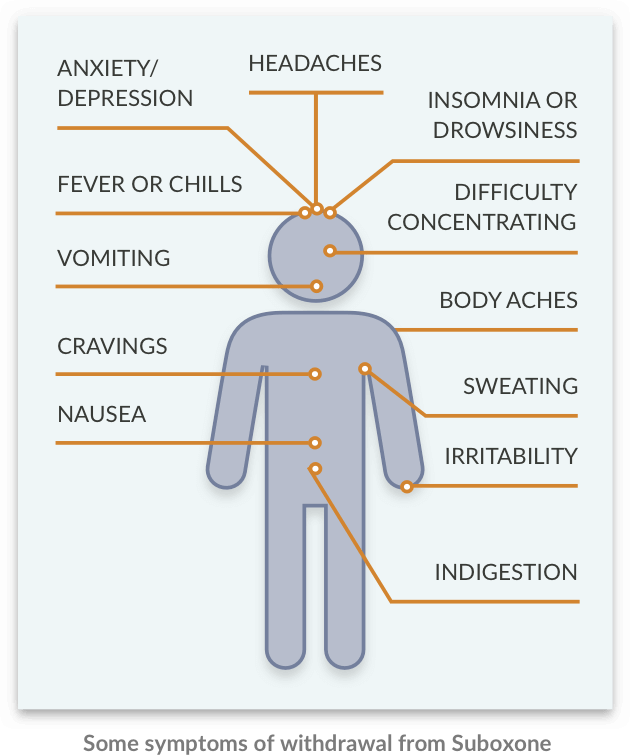
Suboxone Withdrawal Symptoms
Suboxone withdrawal symptoms can last for as long as a month and may include:
- Nausea.
- Vomiting.
- Headaches.
- Muscle aches/body aches.
- Insomnia.
- Lethargy.
- Digestive distress.
- Anxiety.
- Depression.
- Irritability.
- Drug cravings.
- Fever.
- Chills.
- Concentration difficulties.
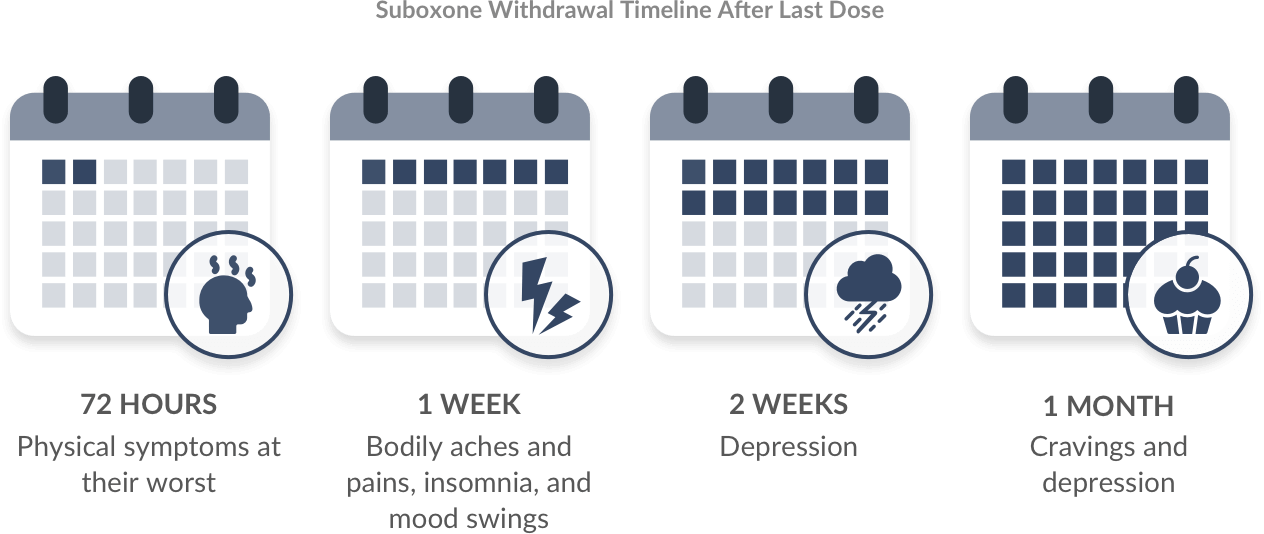
Suboxone Withdrawal Timeline: How Long Do Symptoms Last?
Generally, most physical withdrawal symptoms will subside after 1 month, though psychological dependence can still remain. Symptoms are most significant in the first 72 hours of Suboxone withdrawal. This is when most physical symptoms are experienced. Then, in the first week after discontinuation of Suboxone, symptoms generally subside to general aches and pains in the body, as well as insomnia and mood swings. After the second week, depression is the biggest symptom. After 1 month, individuals will still likely be experiencing intense cravings and depression. This is the most delicate time after stopping Suboxone use, as people have a potential for relapse. As such, the timeline for Suboxone withdrawal is as follows:
- 72 hours: Physical symptoms at most significant.
- 1 week: Bodily aches and pains, insomnia, and mood swings.
- 2 weeks: Depression.
- 1 month: Cravings and depression.
Take Our “Am I Addicted?” Self-Assessment
Take our free, 5-minute “Am I Addicted?” self-assessment below if you think you or someone you love might be struggling with drug or alcohol addiction. The evaluation consists of 11 yes or no questions that are intended to be used as an informational tool to assess the severity and probability of a substance use disorder. The test is free, confidential, and no personal information is needed for the result.
Therapeutic Support and Recovery
One of the keys to maintaining sobriety for the long-term is behavioral therapy. Without it, it may difficult to remain abstinent. Depending on the experience of the patient leading up to and during addiction, and goals for the future, the therapeutic choices incorporated into an individualized treatment plan may vary widely from person to person. In most cases, however, a therapeutic treatment plan to address opioid addiction may include:2
- Evaluation and assessment: A full understanding of all the issues that play a role in a person’s use of drugs is essential to creating a directed and effective treatment plan. Behavioral disorders, co-occurring mental health disorders, underlying medical conditions, trauma, and more are identified early on in order to ensure that these issues are all addressed during the treatment process.
- Unique treatment plan: Depending on the results of the evaluation and assessment, the person’s goals for recovery, length of time in treatment, and available resources, a unique treatment plan is created.
- Personal therapy: Meeting regularly with a therapist on a one-on-one basis can provide a “home base” for the client throughout recovery. Here, it is possible to work on past issues and present challenges, and manage treatment goals.
- Individualized case management: Case management is required to ensure that all pieces of the puzzle are fitting together in a way that provides coping skills for a long and stable recovery after treatment.
- Group therapy sessions: Meeting regularly with others who are also on the path to balance in sobriety can provide a valuable network of support during treatment and in the months and years following.
- Peer support, or 12-Step, meetings: The 12-Step treatment structure has proven beneficial in the lives of millions of people, and many treatment programs incorporate the philosophy and group session style into their programs. This not only offers clients positive support in recovery but also provides them with a portable therapy option that will assist them in the transition into independent sobriety.
- Alternative therapies: Artistic therapies, food-based therapies, exercise therapies, animal-assisted therapies, and more can be excellent additions to the traditional therapies mentioned above.3 These should be selected based on a patient’s interests and areas of need. For example, those struggling with making positive connections with other people in recovery and trusting themselves may opt for a sports and adventure therapy that takes them into the outdoors with a group to explore nature and step outside their comfort zone.
- Holistic therapies: Holistic therapies can also be personalized to suit the personality and interest of the individual. Some popular options include yoga, meditation, music, hypnotherapy, acupuncture, and more.
- Long-term aftercare and support: Treatment does not stop when rehab ends. Rather, this initial phase of recovery is just a starting point, and those who are most successful in maintaining sobriety for the long-term are the ones who remain actively engaged in treatment for years after transitioning into independent living. These aftercare activities can involve continuing to meet with a personal therapist, attending 12-Step meetings, connecting with other support group options, and engaging in holistic and alternative therapies that are meaningful.
How to Cope With Withdrawal Symptoms
There are a wide variety of coping strategies to deal with the stress of withdrawal. These are strategies that can be used when coping with any kind of stress. Rather than engaging in maladaptive behaviors, such as drug or alcohol use, individuals who engage in positive coping behaviors will be able to better maintain recovery.
Some coping mechanisms for Suboxone withdrawal symptoms besides medications include:
- Social activity: Keeping in touch with close family and friends, even without having to tell them about possible withdrawal symptoms and the recovery process, may help provide you with the emotional support you’ll need to make it through detox.
- Relaxation time or hobbies: Making time to relax in the midst of everyday life can be hard, but it is absolutely necessary for maintaining recovery. Many who are suffering from withdrawal may struggle with relaxing in a healthy way, but finding any appealing hobby (writing, art, crafts, etc.) can help you to avoid relapsing back to substance use.
- Adapting to the situation: Accepting that withdrawal is part of the recovery process is important. Adopting a more positive outlook to the recovery process could help to replace feelings of shame, anger, and depression with feelings of satisfaction and pride.
If you or someone you love is struggling with opioid addiction and would like to learn more about inpatient or outpatient treatment, contact an admissions navigator today. An American Addiction Centers (AAC) admissions navigator can talk to you about your options for rehab, detox, and addiction treatment medications. Call