Does Medicaid Cover Drug and Alcohol Rehab?
Does Medicaid Cover Alcohol Rehab or Treatment for Drug Use?
Yes, Medicaid does often cover alcohol rehab and treatment for drug misuse. While individual plans and benefits vary by provider and state, Medicaid plays a major role of financing substance use disorder treatment in the United States.
The Mental Health Parity and Addiction Equity Act was established to ensure that Americans with mental health issues and substance use disorders could receive the care they need by prohibiting discriminatory practices that could limit insurance coverage for behavioral health treatment.12 Federal guidelines now require Medicaid to comply with parity requirements and allow coverage for mental health and SUD to be no less restrictive than coverage that is available for other medical conditions.12
Medicaid Detox Programs
There are detox centers that take Medicaid throughout the country. State-funded detox and rehab programs provide services at a lower cost than private facilities. They are funded by state and federal programs, grants, and tax dollars, and they often accept Medicaid.13 These facilities are essential to the treatment of and recovery from substance use disorders for people who cannot afford private programs, which may cost thousands of dollars per day. Both residential facilities and outpatient treatment programs are available through state-funded programs.13
Medicaid Inpatient Rehab
In 2015, the Obama administration issued guidance to outline how states could potentially cover inpatient rehab and residential treatment for substance use disorders to ensure a comprehensive continuum of care as outlined by the American Society of Addiction Medicine (ASAM).3
The ASAM levels of care encompass early intervention, outpatient services, intensive outpatient treatment, partial hospitalization services, inpatient services, and medically-managed intensive inpatient treatment.
Medicaid Outpatient Rehab
States can use Medicaid’s rehabilitation services option to cover some outpatient treatment for substance use disorders.3 Outpatient treatment options like addiction treatment medications, counseling, and case management can allow for people in recovery to continue to work and care for their families.
Medicaid for Mental Health Counseling and Substance Misuse Therapy
All state Medicaid programs provide some mental health services, and many provide services for substance use disorders as well.2 They typically include therapy, counseling, addiction treatment medications, peer services, and various levels of care for addiction treatment.2
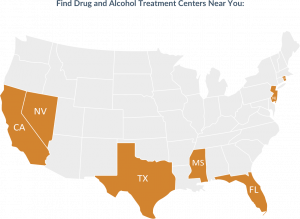
Find Drug and Alcohol Rehab Centers Near You
Are Addiction Treatment Medications Covered by Medicaid?
In 2020, the federal government issued guidelines for states to increase access to medications for addiction treatment, also known as MAT, for opioid use disorders. States are now required to provide Medicaid coverage for certain drugs, counseling, and behavioral therapy.14
Some of the more common addiction treatment medications used for opioid use disorders are:15
- Methadone: An opioid agonist, it acts on opioid receptors in the brain more slowly and without producing the euphoric effects of opioids like heroin. Methadone helps by reducing withdrawal symptoms and cravings.
- Buprenorphine: A partial opioid agonist, it also acts on the opioid receptors in the brain, but is not as strong as methadone and can be taken outside of an approved treatment facility. It helps reduce withdrawal symptoms and cravings.
- Naltrexone: An opioid antagonist, it works differently than methadone or buprenorphine. Naltrexone blocks opioid receptors in the brain and prevents any opioid drug from producing euphoric effects.
Length of Rehab Stay Covered by Medicaid
The length of time a person spends in rehab depends on their individual needs as well as their specific provider benefits. There is no predetermined length of treatment that applies to everyone. However, evidence indicates that treatment outcomes are contingent on adequate treatment length.13
Each state has different rules for eligibility and treatment coverage for Medicaid inpatient rehab. Prior to the ACA, addiction treatment services were often not covered by private insurance and were extremely limited for people with public insurance.16 Insurance companies now have to provide a full range of treatment services, including residential treatment for substance use disorders.16
Inpatient treatment can last anywhere from 5-7 days for medical detox and up to 90 days or more depending on a person’s needs and how they progress in treatment. Outpatient care can last a year or more.17
Does Medicaid Cover Out-of-State Rehab?
The amount of coverage for residential services or outpatient treatment that Medicaid will cover varies by state. You can call any treatment facility to determine if your insurance is accepted, as each state has different eligibility requirements.
Other Rehab Insurance Options
It is possible to have Medicaid supplement private insurance. In most cases, Medicaid acts as the “payer of last resort” for services. Generally, other responsible sources of payment are required to pay for medical costs before Medicaid will do so.19
As requirements can vary substantially from state to state, it will be imperative to work with individual treatment centers to determine what services are covered through individual policies and how much they will cost.
American Addiction Centers offers evidence-based addiction treatment throughout the United States, including inpatient and outpatient rehab, behavioral therapy, addiction treatment medications, and aftercare. We offer various payment options – which might be able to be combined – to help you pay for care. To learn more, verify your insurance coverage now or call
- Medicaid.gov. (2024). Medicaid.
- Medicaid.gov. (n.d.). Behavioral Health Services.
- Bailey, A., Hayes, K., Katch, H., Solomon, J. (2021). Medicaid is Key to Building a System of Comprehensive Substance Use Care for Low-Income People, Center on Budget and Policy Priorities.
- National Conference of State Legislatures. (2011). Medicaid and the Affordable Care Act.
- Medicaid.gov. (2021). Substance Use Disorders.
- United States Senate: Committee on Finance. (2022, March). Mental Health Care in the United States: The Case for Federal Action.
- Substance Abuse and Mental Health Services Administration. (2020). National Survey of Substance Abuse Treatment Services: 2020
- Medicaid.gov. (n.d.). Eligibility.
- Healthcare.gov. (2025). Federal poverty level (FPL).
- U.S. Department of Veteran Affairs. (2020). VA Healthcare and Other Insurance.
- Center on Budget and Policy Priorities. (2020). Taking Away Medicaid for Not Meeting Work Requirements Harms Veterans.
- Medicaid.gov. (n.d.). Parity.
- National Institutes of Health. (2018). Principles of drug addiction treatment: A research-based guide (third edition).
- Department of Health & Human Services: Centers for Medicare & Medicaid. (2020, December 30). Mandatory Medicaid State Plan Coverage of Medication-Assisted Treatment.
- National Institute on Drug Abuse (NIDA). (2018). Opioid Agonists and Partial Agonists (Maintenance Medications.
- Abraham, A., Andrews, C., Grogran C., Daunno, T., Humphreys, N., Pollack, H., Friedmann, P. (2017, January). The Affordable Care Act Transformation of Substance Use Disorder Treatment. National Center for Biotechnology Information (NCBI).
- Lesser, B. (2021). How Long Should Rehab Stay Be?
- Congress.gov. (2018). The SUPPORT for Patients and Communities Act.
- Medicaid and CHIP Payment and Access Commission. (n.d.). How Medicaid Interacts with Other Payers.
- Healthcare.gov. (n.d.). Medicaid and CHIP program names in your state.
Rehabs That May Accept Medicaid Insurance
Frequently Asked Questions
What is the difference between Medicaid and Medicare?
What is Medicaid called in my state?
| State | Alternative Name |
|---|---|
| Alabama | - |
| Alaska | DenaliCare |
| Arizona | Arizona Health Care Cost Containment System (AHCCCS) |
| Arkansas | - |
| California | Medi-Cal |
| Colorado | Health First Colorado |
| Connecticut | HuskyHealth |
| Delaware | Diamond State Health Plan (Plus) |
| Florida | Statewide Medicaid Managed Care Program |
| Georgia | - |
| Hawaii | MedQuest |
| Idaho | - |
| Illinois | Medical Assistance Program |
| Indiana | Hoosier Healthwise Hoosier Care Connect M.E.D. Works Health Indiana Plan (HIP) Traditional Medicaid |
| Iowa | IA Health Link |
| Kansas | KanCare Medical Assistance Program |
| Kentucky | - |
| Louisiana | Bayou Health HealthyLouisiana |
| Maine | MaineCare |
| Maryland | Medical Assistance |
| Massachusetts | MassHealth |
| Michigan | Medical Assistance or MA |
| Minnesota | Medical Assistance (MA) / MinnesotaCare |
| Mississippi | Mississippi Coordinated Access Network (MississippiCAN) |
| Missouri | MO HealthNet |
| Montana | - |
| Nebraska | ACCESSNebraska |
| Nevada | - |
| New Hampshire | - |
| New Jersey | New Jersey FamilyCare |
| New Mexico | Centennial Care |
| New York | Medicaid Managed Care |
| North Carolina | Division of Medical Assistance (DMA) |
| North Dakota | North Dakota Medicaid Expansion Program |
| Ohio | - |
| Oklahoma | SoonerCare |
| Oregon | Oregon Health Plan |
| Pennsylvania | Medical Assistance (MA) |
| Rhode Island | RI Medical Assistance Program |
| South Carolina | Healthy Connections |
| South Dakota | - |
| Tennessee | TennCare |
| Texas | - |
| Utah | - |
| Vermont | Green Mountain Care |
| Virginia | - |
| Washington | Apple Health |
| Washington D.C. | Healthy Families |
| West Virginia | - |
| Wisconsin | ForwardHealth / BadgerCare |
| Wyoming | EqualityCare |
How long does it take to get covered by Medicaid?
Finding a rehab near me that may take Medicaid
- All Treatment Centers: See All Rehabs
- California: Laguna Treatment Center
- Florida: Recovery First Treatment Center
- Florida: River Oaks Treatment Center
- Las Vegas: Desert Hope Treatment Center
- Locations Nationwide: Resolutions Recovery Residences
- Massachusetts: Adcare Treatment Hospital
- Mississippi: Oxford Treatment Center
- Rhode Island: Adcare – Outpatient
- Rhode Island: Adcare – Inpatient
- Texas: Greenhouse Treatment Center