Veteran Addiction: Veteran Drug & Alcohol Rehab Near Me
Veterans returning home from military deployment and combat may face a number of challenges when trying to adjust back to civilian life.
Arguably, one of the biggest challenges is coping with any traumas they may have endured during deployment, such as significant injury, witnessing the death of a peer, or sexual assault.
The rates of post-traumatic stress disorder (PTSD) are high for Veterans, specifically for those in the Army or Marine Corps who experienced moderate to severe combat. These Veterans may also show signs of other mental health issues, drug abuse, and other physical health issues relating to the traumas they experienced during their military service.
Confidential, toll-free, 24/7 phone number.
Our admissions navigators are always available to assist you.
Call now.
Additionally, American Addiction Centers (AAC) works with Veterans Affairs to provide treatment to Veterans through VA benefits. Find out if you qualify below, or download our PDF here to see how our team can help you navigate the VA system.
Veterans and Addiction
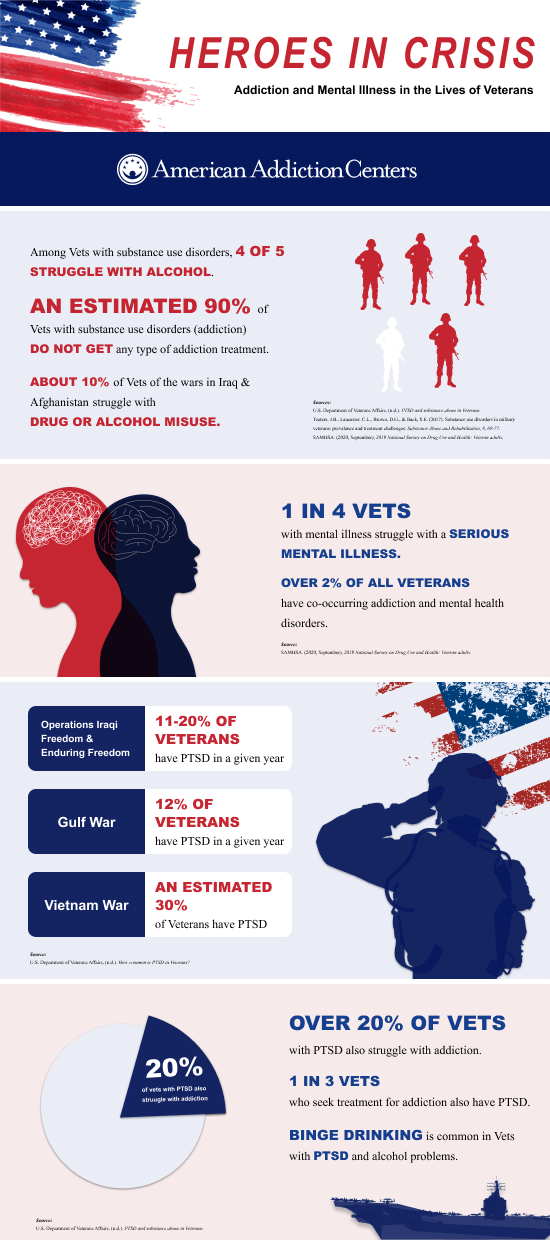
One study found that 11% of Veterans seeking services for the first time from the VA met the criteria for a substance use disorder.2,3
The reasons behind this are complex, but contributing factors include issues such as physical disabilities and mental health problems, as well as the prescribing of addictive opioids for pain and injuries. The trauma of combat may also contribute to substance misuse.4
Veterans who have mental health issues may also hesitate to seek help due to the perceived stigmas surrounding mental health disorders and turn to alcohol and/or other drugs to self-medicate.5
Veteran Stress and Challenges of Civilian Life
Military service, especially deployment to combat zones, is rife with extreme stress. Veterans may come back having witnessed or participated in significantly traumatic events. They may be injured or dealing with issues such as:6,7
- Chronic pain.
- PTSD, depression, or other mental health issues.
- Substance dependence or addiction.
- Homelessness.
Leaving the military and returning to civilian life requires a period of readjustment that can be very challenging and uncomfortable for any Veteran.7 When you add the issues of injury, pain, trauma, and drug or alcohol addiction, it’s easy to see just how many uphill battles a Veteran may face.
Unfortunately, many Veterans may not get the help they need due to an unwillingness or inability to seek help. Without the help they need, they may be at higher risk of suicide.7 The National Institute on Drug Abuse (NIDA) states that suicide rates among Veterans exceed those of the general population.7 In 2020, there were 6,146 Veteran suicide deaths, 343 fewer than in 2019.8
Veteran’s and Alcohol Misuse
Alcohol misuse is common among active-duty Service Members, and unhealthy drinking habits can continue long after military service ends.9
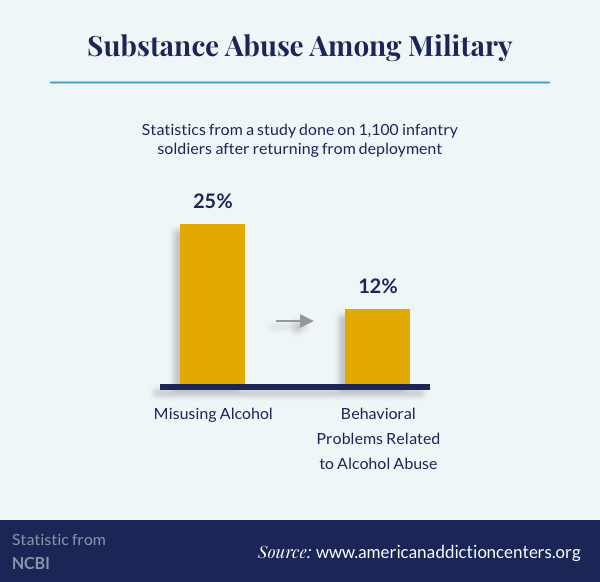
Combat exposure appears to be a major risk factor for alcohol problems in military personnel. A study looking into the alcohol consumption of 1,120 soldiers who had been part of a brigade infantry team returning from deployment found a correlation between combat (especially exposure to threats and atrocities) and alcohol misuse.10 An estimated 25% of those who were sampled were misusing alcohol 3-4 months after deployment.10 Of those, 12% experienced behavioral problems related to their alcohol use.10
Drug Use and Abuse Among Veterans: Statistics and Prevalence
Veterans are at risk of developing a dependence or addiction to opioid painkillers if they obtain a prescription for pain or injury.7 However, there have been efforts to prevent opioid misuse and addiction.
There is evidence to suggest that harm associated with the misuse of prescription opioids can lead to an increased risk of dependence. It has been reported that 2 out of 10 Veterans who have been diagnosed with PTSD are also diagnosed with a substance use disorder (SUD).11
The United States Army released a memo to warn that treating PTSD with benzodiazepines was not worth the risk and that it might worsen the patient’s fear and delay their recovery from trauma.12
Veterans, similar to many civilians, are also at risk for developing substance use disorders. Marijuana accounts for the vast majority of drug use among Veterans.13 Additionally, one government reports that more than 10% of Veteran admissions to substance use treatment centers are for heroin; cocains accounts for approximately 6%.13
Some data suggests that Veterans are more likely to be smokers.14 With the rates of Veterans who smoke (14.6%), health conditions caused by smoking, such as coronary heart disease, lung cancer, and chronic bronchitis are cause for concern.14
Are There VA-Approved Rehab Centers?
AAC works with the VA through the VA Community Care Network. The VA Community Care Network is a network of external physicians, facilities, and practitioners who can provide necessary care to Veterans when the VA is unable to do so. A number of AAC’s rehab facilities partner with the VA through the program. Call us at .
AAC’s Veteran Program

AAC offers many programs focusing on alcohol and substance misuse in our treatment centers across the country. The Veteran program was created specifically for Veterans. AAC offers a variety of Veteran-specific programs, groups, and benefits because we realize the needs of this population are different from others. At our treatment facilities:
- Every Veteran receives a psychosocial assessment as well as a history and physical soon after admission, ensuring any comorbid conditions are identified and treated appropriately.
- Veterans meet with a therapist individually one time per week along with daily check-in sessions.
- Group sessions take place 5 times per day.
- Nightly commitments come from local mutual-help groups.
The Veteran program is a specialized addiction recovery program at our facilities dedicated to military Veterans who have been diagnosed with substance use and other co-occurring mental health disorders.
Serving in the U.S. military can potentially lead to a higher risk for developing substance use and mental health disorders for many individuals, making it difficult to:
- Manage a work/life balance.
- Protect against stress-related disorders.
- Identify the impacts of addiction on themselves and family.
- Connect with the emotions of others.
- Recognize the beginning stages of PTSD.
Our treatment team and healthcare professionals understand the obstacles and difficulties in life, how they can lead to addiction, and the requirements for specialized treatment and unique recovery programs for those with a military background.
The Veteran program is an evidence-based treatment program offering inpatient care that addresses the health and wellness of the entire patient. Treatment can include:
- Family therapy.
- Group work.
- Individual therapy.
- Intensive relapse prevention.
- Life skills.
- Medical stabilization and detoxification with medical monitoring.
- Multidisciplinary assessment and testing.
- Wellness program.
Therapies in the Veteran program focus on helping Veterans create strategies for positive decision-making and lifestyle changes. Here are some of the therapies included in the Veteran program:
- Cognitive Behavioral Therapy (CBT): Patients learn to identify and shift negative thinking patterns, as well as behaviors, to live a healthier and happier life.
- Eye Movement Desensitization and Reprocessing (EMDR): This helps patients find resolutions to traumatic and disturbing events and life experiences.
- Family Systems Theory: This therapy looks at the family as an emotional unit and explores its complexity to help Veterans find their places in the family unit after service.
- Pain Management Group: This teaches Veterans how to addresses and deal with pain and physical injuries from military service.
Insurance Coverage for Veteran and VA Rehab
AAC accepts many insurance providers that are in-network, including TRICARE, to aid in covering treatment programs. TRICARE covers active duty members, Veterans, activated guard and reserve members, and military family members. To learn more about your coverage, call the number found on your insurance card or fill in the form below.
Videos About Veteran Addiction and Rehab
The Veteran Program
Navigating Veteran and VA Benefits
A Veteran’s Treatment Testimonial
Veterans and Mental Health
Between 37% and 50% of Veterans returning from Afghanistan and Iraq have been associated with a mental disorder associated with a substance use disorder.15 As mentioned above, harsh conditions and traumatic events that some service members face during their time in military, it only seems obvious that Veterans could suffer from mental health conditions.
According National Institute of Mental Health, in 2020 about 1 out of 5 adults were living with a mental health condition, ranging from mild to severe.16
Traumatic Brain Injuries
A traumatic brain injury (TBI) is the result of an impact to the head, causing the damage to the brain.17 TBI symptoms include:17
- Behavioral changes.
- Headaches.
- Issues with memory, attention, language, or problem-solving speed.
- Sensitivity to light and noise.
- Sleep impairment.
In addition, Veterans suffering from a TBI can show signs of changes in personality, which can be concerning to family members and loved ones.18
A study published in 2018 from the U.S. Department of Veteran Affairs looked at the connection between TBI and suicidality specifically in veterans who were deployed to Iraq or Afghanistan.19 Research indicates that service members with TBIs have higher rates of PTSD.20 More than 185,000 Veterans, who use the VA for their health care, have been diagnosed with a TBI, the majority of which are mild.20
PTSD and Substance Misuse
PTSD, post-traumatic stress disorder, also referred to as “shell shock” or “combat fatigue,” is a mental health condition that can be a diagnosis for those that have experienced combat, physical or sexual assault, terrorist attack, or serious accidents or disaster.11
Most Veterans that are diagnosed with PTSD have been in combat. More than 2 in 10 Veterans with PTSD also have a SUD.21
Symptoms of PTSD may include:22
- Feeling wound up or jumpy.
- Easily angered and feeling irritated.
- Experiencing flashbacks of the traumatic event.
- Feeling numb to things that use to bring joy.
- Difficulty sleeping or concentrating.
Substance misuse and addiction are commonly connected to co-occurring disorders like PTSD, depression, and anxiety in Veterans.21
Research has found that service members and Veterans that have heavy drinking tendencies are more likely to have PTSD, depression, and suicidal intentions than veterans who drink moderately.30 War veterans with a PTSD diagnosis and alcohol problems tend to binge drink.21
From a study of Operations Enduring Freedom/Iraqi Freedom/New Dawn, 63% of Veterans were diagnosed with PTSD and an alcohol use disorder (AUD) or SUD.23 In addition, of the Veterans diagnosed with PTSD and AUD, over 36% were also diagnosed with major depression, 43.5% were diagnosed with an anxiety disorder, 39% had suicidal intentions, and 46% attempted suicide.23
Substance Misuse can Lead to Suicide
The combination of trauma, mental health disorders, and substance misuse exacts a very real toll on Veterans. In 2020, 6,146 Veterans committed suicide—about 17 Veterans a day. This was a decrease of 343 Veterans from 2019.8
Supporting Veterans with Addiction and Co-Occurring Diagnosis
Mental health issues and addiction can affect your family and the people around you. With a diagnosis of PTSD and addiction, seeking treatment and medical care is the first step.
Family members and loved ones need to be encouraging and possibly willing to change some of their habits and behaviors that may present a risk for the Veteran with addiction and a co-occurring diagnosis.24 For family members and loved ones, it is important to learn more about addiction and co-occurring issues to provide support to the Veteran in their lives.24
Chronic Pain and Physical Traumas Affecting Veterans
Due to the extreme physical demands that most service members have endured, chronic pain and physical pain are common issues for Veterans.25 Most treatment options for acute and chronic pain are prescription medications combined with physical therapy such as yoga or chiropractic care.26
Those who experience chronic pain and physical traumas are often prescribed opioids, which are highly addictive drugs. Patients on a prolonged prescription of opioids can develop opioid dependence.27 The VA continues to address the opioid epidemic in the United States through education and awareness of the harm opioids can have on active-duty and Veteran patients.
Chronic Pain
Chronic pain can be the root cause of disabilities, with a decrease in work productivity.28 Persistent chronic pain can contribute to mental health issues, such as depression, anxiety, loss of quality sleep, decreased quality of life, and substance abuse.28
Acute and chronic pain can be the result of injuries to the spinal cord or back, burns, traumatic brain injuries, and cancer.28
Over 65% of Veterans have a chronic pain diagnosis, while 9.1% suffer from severe pain.28 As many as 40% of Veterans over the age of 65 are diagnosed with chronic back pain.28 Spinal injuries are a common cause for chronic pain and nerve pain, which can be very difficult to treat.28
Researchers are still studying the treatment options to best help those with chronic pain.28 The VA is currently learning more about chronic pain, specifically nerve pain, at the Center for Restoration of Nervous Systems Function at Yale School of Medicine.28
Sexual Assault Trauma
Military sexual trauma is a term used to describe a service member, regardless of gender, who had experienced sexual assault or sexual harassment while serving in the military.29 About 1 in 5 female Veterans have been diagnosed with military sexual trauma by the VA.30 Veterans who have experienced sexual trauma may display the following symptoms:29
- Misuse of substances or alcohol.
- Difficulty feeling safe.
- Depressed or numb.
- Experiencing disturbing memories or nightmares.
- Feeling isolated from others.
- Sleeping problems.
In addition to military sexual trauma diagnosis, active-duty and Veteran members of the military can be diagnosed with PTSD after a sexual assault.31 A preliminary study indicated that female Veterans with PTSD were likely to have been sexually abused during their time in service.31 The same study also indicated that these female Veterans were more likely to misuse substances to help cope with their trauma and PTSD.31
Reducing Stigma of Veteran Addiction & Substance Abuse

There are still stigmas about mental health and substance misuse in the military for both service members and Veterans. Because of this, many do not seek treatment and go undiagnosed. In these cases, Veterans with addiction and other untreated mental health disorders can negatively affect those around them and cause harm to themselves.
Veterans who are seeking treatment may decide not to go due to the social stigmas that surround mental health and addiction in service members and Veterans.32 Many Veterans worry about the negative perception others may have about them if they address their mental health issues and addiction.32
The U.S. Department of Defense is aware of the stigmas that may stop a service member or Veteran from seeking treatment. In their efforts to combat these stigmas, the U.S. Department of Defense launched an anti-stigma campaign in 2009 called the Real Warriors. Real Battles. Real Strength. The campaign encourages active-duty service members and Veterans to seek help and learn more about their “invisible wounds,” such as alcohol use disorder, drug misuse, and mental health issues.
Veteran and Veteran Rehab Support Organizations
There are many government-funded, nonprofit, and community groups and organizations that focus on helping Veterans live healthy lives after serving in the military.
The VA healthcare system provides information about Veteran benefits and medical care. More information can be found on VA.gov. Veterans can log in to My Health and set up substance abuse screenings.
In addition to setting up screenings and healthcare appointments, Veterans and their families can learn more about substance misuse, mental health conditions, and treatment options on the VA’s website. Veterans and their families can also contact the following for more information:
- Help for Homeless Veterans: 877-424-3838
- Caregiver Support: 855-260-3274
Helping Veterans with Addiction
Addiction can affect the lives of family members and loved ones. For friends and family members, there are things you can do to support someone in your life with an addiction.
By recognizing the signs of addiction, learning more about interventions, researching treatment options, and providing support and understanding, you can help those in your life recover.
Recognizing the Signs of Substance Abuse
For family members and close friends of Veterans, there are numerous signs for someone suffering from PTSD or other mental health issues, substance misuse, or a combination of the two.
Veterans experiencing substance misuse, specifically drugs, may experience:
- Problems at work, such as poor performance, poor time management, and social dysfunction.
- Lack of motivation or energy.
- Neglecting relationships with friends and family.
- Obsession or strong cravings for substance.
- Experiencing withdrawal symptoms.
When there are signs of substance misuse, family members should be encouraged to address the situation with a loved one.
Alcohol use disorder and drug addiction affects many active service members and Veterans. For families and close friends, providing support and learning more about addiction and treatment options can make the difference in a Veteran’s recovery. The information in this guide and treatment options offered at AAC can help Veterans with addiction and co-occurring mental health issues recover and live a life of sobriety.
