Drug Withdrawal Symptoms, Timelines & Treatment
According to the Centers for Disease Control and Prevention, in 2018, more than 11% of Americans ages 12 and older used illicit substances within the month before being surveyed.1
Many abused drugs are associated with the development of significant physiological dependence—especially when consistently consumed in large amounts. When substance dependence develops, people may be at risk of experiencing unpleasant withdrawal symptoms when trying to stop drinking or using drugs.
What Is Drug Withdrawal?
Drug withdrawal is a physiological response to the sudden quitting or slowing of use of a substance to which the body has grown dependent on. The various types of drug withdrawal syndromes may involve different combinations of physical, mental, and emotional symptoms—some of which can prove dangerous if left unmanaged.
Symptoms of Withdrawal
The symptoms of withdrawal from substances may be different depending on the substance used. Common symptoms of withdrawal may include:
- Trembling and tremors
- Muscle pain or aches
- Hunger or loss of appetite
- Fatigue
- Sweating
- Irritability and agitation
- Depression
- Anxiety
- Nausea
- Vomiting
- Confusion
- Insomnia
- Paranoia
- Seizures
- Dilated pupils
Why Does Withdrawal Occur?
When someone regularly drinks alcohol or uses certain drugs, their brain may begin to adjust to the presence of these substances. They may eventually become physiologically dependent on their substance of choice and utterly reliant on it to function and feel “normal.”
In people who develop significant levels of dependence, withdrawal is often an inevitable response to the sudden absence or declining blood concentration of a given substance. Withdrawal symptoms may develop when a substance-dependent person quits a substance “cold turkey” or substantially reduces how much they are using. During withdrawal, the body attempts to reach a new state of homeostasis as it rids itself of any lingering chemical influence of the drug in question. This can result in temporary disruptions in brain chemistry and may be accompanied by significant mental and physical health repercussions.
Can Withdrawal Be Lethal?
If not medically managed, withdrawal from certain substances, such as alcohol and benzodiazepines, can be quite severe and, in some cases, lethal. But it’s rare.
For instance, severe alcohol withdrawal is sometimes associated with a syndrome known as delirium tremens. If not recognized and appropriately managed, delirium tremens can progress to severe seizures and potential death. Some estimates point to the condition being present in fewer than 5% of people who experience alcohol withdrawal. It is, however, fatal in about 15% of those alcohol withdrawal cases without treatment.2
Though opioid withdrawal symptoms are seldom life-threatening, they can be intensely uncomfortable. And though the symptoms themselves may not be lethal, one significant risk for those attempting to opioid withdrawal without medical assistance is returning to opioid use. Should this happen after a long enough duration of abstinence that opioid tolerance has significantly decreased, people may be at a heightened risk of overdose.3,4
In such situations, medical detox—where a team of doctors and nurses can help manage withdrawal symptoms, alleviate discomfort, and minimize the risk of dangerous withdrawal complications—can be immensely helpful in early recovery and has the potential to ultimately save lives.
Does insurance cover withdrawal treatment?
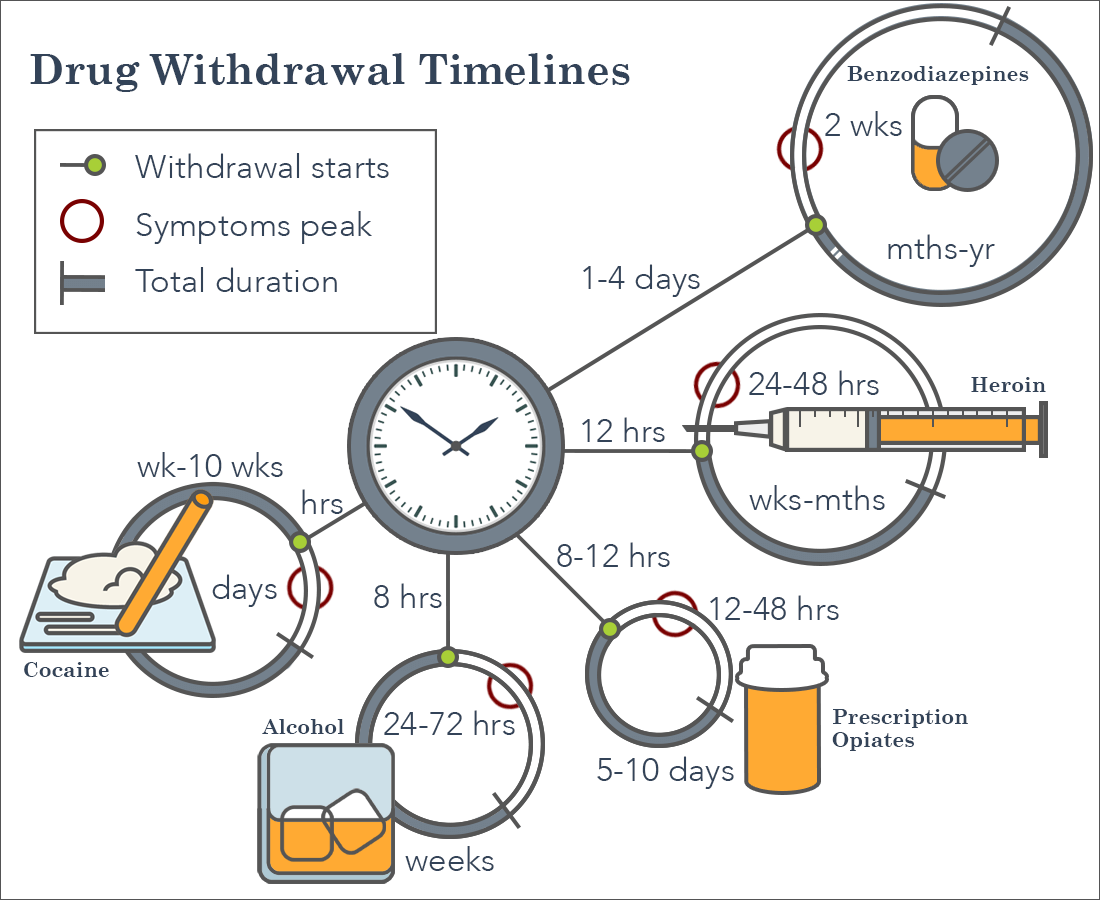
Drug Withdrawal Timelines: How Long Does Withdrawal Last?
The precise duration of withdrawal is influenced by which substance someone used as well as the magnitude of their dependence on the substance. It may take days, weeks, and—in some cases—months to reach complete resolution of all withdrawal symptoms, depending on various factors and individual differences.
A general overview of certain drugs and their characteristic withdrawal timeline is as follows:
-
- Alcohol: The first signs of alcohol withdrawal may appear within several hours after the last drink and peak over the course of 24-72 hours.5 Delirium tremens usually develops 48-72 hours after heavy drinking stops and usually lasts for 3-4 days but can last up to 8 days.6
- Short-Acting Opioids (such as heroin and certain prescription painkillers): Short-acting opioid withdrawal symptoms generally begin 8-24 hours after last use and last an average of 4-10 days.
- Longer-acting opioids (such as methadone): For methadone and other longer-acting opioids, it may take 2-4 days for withdrawal symptoms to emerge. Withdrawal will likely fade within a period of 10 days.7
- Benzodiazepines (such as Xanax and Valium): Withdrawal from benzos may begin within 1-4 days after the last use, peaking in severity in the first 2 weeks. In some cases, certain symptoms of protracted withdrawal can remain troublesome for months or years without treatment.8
The severity and duration of withdrawal from substance dependence are contingent upon many factors, including the amount of a drug that someone used and how frequently they used it. Unfortunately, withdrawing from drugs is often a profoundly uncomfortable experience that can stall or otherwise complicate recovery efforts.
Alcohol Withdrawal
People with significant alcohol dependence may be at risk of severe withdrawal and should not attempt to quit alcohol “cold turkey” because of the increased likelihood of seizure development or other withdrawal-associated complications. For many, alcohol withdrawal is uncomfortable, but in some instances, it can also prove life-threatening if not appropriately managed through medical detox efforts.
Alcohol is a central nervous system depressant, or CNS depressant, and abruptly quitting or slowing use after developing dependence can result in potentially dangerous nervous system excitation as the body restores equilibrium. Alcohol withdrawal symptoms may arise within hours of the last drink. Still, some of the more serious risks remain a factor for several days.
Symptoms of Withdrawal for Alcohol
Individuals who are dependent on alcohol may experience some of the following distressing alcohol withdrawal symptoms when trying to quit:2,9
- Elevated blood pressure
- Racing pulse
- Sweating
- Insomnia
- Tremors
- Anxiety
- Agitation
- Headache
- Sweating
- Nausea/vomiting
- Hallucinations
- Seizures
It is not always that straightforward to predict who is at the highest risk for severe withdrawal and withdrawal complications. However, the likelihood of experiencing significant withdrawal increases with the average quantity and frequency of drinking. People with certain concurrent medical issues, a history of polysubstance use, and those who have experienced previous episodes of alcohol withdrawal may be at additional risk.
While alcohol withdrawal can start within the first few hours after the last drink, delirium tremens may not start until a few days later, and appear suddenly, making alcohol withdrawal safest when monitored around the clock by medical professionals.
Heroin & Opiate Withdrawal
Heroin belongs to the opioid class of drugs. Opioids work by attaching to and activating opioid receptors throughout the body. Opioid receptor activation is associated with a subsequent release of dopamine in the brain, which serves to reinforce the continued use of opioid drugs for their pleasurable effects.10
Opioids are a widely abused and highly addictive class of drugs. Some degree of opioid dependence may develop after short periods of use, even when taken according to a prescription, in the case of prescription painkillers.
Opioid medications, when used under the supervision of a medical doctor, successfully alleviate physical pain caused by injury, illness, or surgery. Misuse of these drugs can greatly increase the risk of someone becoming physiologically dependent on them.
Symptoms of Withdrawal for Opioids
The acute opioid withdrawal syndrome may include several characteristic symptoms, such as:8,11
- Nervousness or anxiety.
- Trouble sleeping.
- Frequent yawning.
- Nausea.
- Diarrhea.
- Flu-like symptoms.
- Muscle cramps/body aches.
- Runny nose.
- Excessive sweating.
- Hot and cold flashes.
- Goosebumps.
Although withdrawal from heroin and other opioids is rarely associated with life-threatening complications, enduring the sometimes markedly unpleasant symptoms can present unnecessary challenges to recovery. The mere discomfort of withdrawal—which some describe as mimicking a bad case of the flu—can lead to immense physical and psychological distress.11
Left unmanaged, opioid withdrawal can easily drive someone toward immediate relapse, which can derail recovery attempts.
Benzodiazepine Withdrawal
Benzodiazepines, or “benzos” as they are sometimes referred to, are a class of drugs that effectively treat anxiety, panic disorder, and certain types of seizure disorders.
These medications are CNS depressants and work on the brain by increasing activity at receptors for the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). This increase in GABA activity also increases inhibition of brain activity, producing a drowsy or calming effect that may be medically beneficial.12
Some widely prescribed benzodiazepines include:
- Xanax.
- Ativan.
- Klonopin.
- Valium.
Symptoms of Withdrawal for Benzodiazepine
Potential symptoms of benzo withdrawal may include:
- Anxiety.
- Agitation.
- Sweating.
- Increased heart rate.
- Trouble sleeping.
- Nausea and/or vomiting.
- Hallucinations.
- Seizures.
When used as prescribed under the care of a physician, benzos can help many people manage anxiety, panic, and certain other conditions. However, misuse increases the risk of developing significant dependence on these drugs.
Cocaine Withdrawal
Cocaine is an exquisitely addictive stimulant drug that influences the brain’s reward center by blocking the removal of dopamine from the synapses.13 This effect in the brain reinforces cocaine use and lays the groundwork for eventual compulsive patterns of use. In turn, this can drive the development of physiological dependence to the drug.
When someone abruptly stops using cocaine, they may experience a severe, negative change in their mood. A dependent user may experience cocaine withdrawal within the first day of their last use, and their withdrawal symptoms could last weeks.
Symptoms of Withdrawal for Cocaine
Cocaine withdrawal is rarely physically dangerous, but may include several distressing psychological symptoms, such as:
- Depressed mood.
- Ongoing tiredness or lethargy.
- Insomnia or hypersomnia.
- Anxiety.
- Irritability.
- Paranoia.
- Increased appetite.
- Problems with concentration.
- Slowed thoughts and movements.
- Intense drug craving.
Withdrawal Treatment: When Is Drug Detox Necessary?
There are certain factors to consider when deciding whether someone should seek medical detox to manage withdrawal.
Withdrawal can be challenging—and sometimes dangerous—for someone who is first getting sober. If you’re thinking of getting sober, it’s recommended that you seek guidance from a medical professional, who may recommend a medical detox. This way, once withdrawal symptoms appear, they can be managed appropriately by trained medical staff. Withdrawal management is a large part of the medical detox process. It refers to the medical and psychological care of patients who are experiencing withdrawal symptoms as a result of stopping or significantly reducing use of the drug with which they developed a dependence.11
With many substances, medical detox provides the safest, most comfortable setting for withdrawal management. While in detox, patients can safely rid their bodies of the toxic influence of substances under the care of medical professionals, who can monitor vital signs, such as high body temperature or high blood pressure, and administer medications to prevent or manage severe symptoms.
The goal of detox is to reach a state of safety and a comfortable level of mental and physical stability. Someone addicted to alcohol, opioids, benzodiazepines, and other sedatives commonly benefit from undergoing medical detox to safely manage withdrawal with the fewest number of adverse consequences. Many facilities also offer same-day admission detox for cases that need attention sooner rather than later.
Take Our “Am I a Drug Addict?” Self-Assessment
Take our free, 5-minute “Am I a Drug Addict?” self-assessment below if you think you or someone you love might be struggling with drug addiction. The evaluation consists of 11 yes or no questions that are intended to be used as an informational tool to assess the severity and probability of a substance use disorder. The test is free, confidential, and no personal information is needed to receive the result.
How Long Does Detox Last?
Most patients will complete a drug detox program in a couple days to a week. How long drug detox lasts depends upon a variety of factors, including which drugs someone used, how much of the drug was used, how long the person has been using, as well as the person’s overall health. Typically, detox is the first step of treatment, and patients will enter rehab and therapy to learn coping and recovery techniques.
What Are The Medications Used In Drug Detox?
To stabilize someone in withdrawal from certain substances at the start of a longer-term treatment for substance use disorders (SUDs), medical professionals may administer different medications to ease symptoms and decrease the risk of complications.
For example, some medications that may be used during opioid detox include:11
- Clonidine: A medication used to lessen certain symptoms of opioid withdrawal, including anxiety, tremor, sweating, and chills.
- Lofexidine: A recently approved medication in the same class as clonidine used similarly to reduce certain opioid withdrawal symptoms.14
- Buprenorphine: An FDA-approved partial opioid antagonist medication used to treat opioid use disorder (OUD) that controls cravings and lessens withdrawal symptoms.
- Methadone: A long-acting, full opioid antagonist medication used to stabilize and maintain people in recovery from OUD.
Medications for alcohol and sedative withdrawal management may include:
- Benzodiazepines, which are commonly administered for the management of acute alcohol withdrawal, for seizure prophylaxis, and other symptomatic management, before being tapered off throughout the detox period.9
- A relatively long-acting benzodiazepine (e.g., diazepam) will first be substituted for the benzodiazepine previously used if the individual has benzodiazepine dependence. Then, it will be tapered slowly to ease withdrawal over a more extended amount of time.8
Different drugs have varying withdrawal timelines, symptoms, and risks. Treatment must be individually tailored to treat withdrawal from the specific drug, or drugs, to which someone has developed dependence.
One of the primary goals of medical detox is to facilitate continued, longer-term treatment efforts after the withdrawal period has been successfully managed. Detox, though often hugely important, is not a substitute for additional rehabilitation efforts. Comprehensive rehab care can take place in a residential/inpatient or outpatient setting, depending on individual needs. No matter what the setting, formal substance use treatment commonly begins with a period of detox, followed by ample behavioral therapeutic interventions and continued medical care, as needed.

